RBSE Class 12 Biology Important Questions Chapter 3 Human Reproduction
Rajasthan Board RBSE Class 12 Biology Important Questions Chapter 6 Molecular Basis of Inheritance Important Questions and Answers
Rajasthan Board RBSE Solutions for Class 12 Biology in Hindi Medium & English Medium are part of RBSE Solutions for Class 12. Students can also read RBSE Class 12 Biology Important Questions for exam preparation. Students can also go through RBSE Class 12 Biology Notes to understand and remember the concepts easily. Browsing through manav janan class 12 in hindi that includes all questions presented in the textbook.
RBSE Class 12 Biology Chapter 3 Important Question Human Reproduction
Multiple Choice Questions
Question 1.
Which one is primary sex organ?
(a) Penis
(b) Scrotum
(c) Testis
(d) Prostate
Answer:
(c) Testis

Question 2.
The testes are abdominal in:
(a) elephant
(b) goat
(c) kangaroo
(d) rabbit
Answer:
(a) elephant
Question 3.
Testes are masses of coiled:
(a) uriniferous tubules
(b) malpighian tubules
(c) seminiferous tubules
(d) vasa efferentia
Answer:
(c) seminiferous tubules
Question 4.
Sperms are produced in:
(a) vas deferens
(b) interstitial cells
(c) seminiferous tubules
(d) prostate gland
Answer:
(c) seminiferous tubules
Question 5.
A primary spermatocyte is:
(a) haploid
(b) diploid
(c) polyploid
(d) aneuploid
Answer:
(b) diploid
Question 7.
Testosterone is secreted by which endocrine part of testis?
(a) Cells of Ley dig
(b) Seminiferous tubules
(c) Tunica albugenia
(d) Sertoli cells
Answer:
(c) Tunica albugenia
Question 6.
Failure of descending testis into the scrotum is known as:
(a) paedogenesis
(b) castration
(c) cryptorchidism
(d) impotence
Answer:
(a) paedogenesis
Question 8.
Cervix is situated between:
(a) Oviduct and uterus
(b) Vagina and uterus
(c) Clitoris and labia
(d) Vagina and cletoris
Answer:
(b) Vagina and uterus
Question 9.
The number of embryonic membranes in human is:
(a) 2
(b) 3
(c) 4
(d) 0
Answer:
(c) 4
Question 10.
Menstruation occurs due to:
(a) increased level of luteinizing hormone
(b) decreased level of follicle-stimulating hormone
(c) decreased level of estrogen and progesterone
(d) None of these
Answer:
(c) decreased level of estrogen and progesterone
Question 11.
Human placenta is:
(a) haemochorial
(b) syndesmochorial
(c) yalk sac
(d) haemoendothelial
Answer:
(a) haemochorial
Question 12.
In human females, Meiosis-II is not completed until:
(a) uterine implantation
(b) birth
(c) puberty
(d) fertilization
Answer:
(d) fertilization
Question 13.
The formation of archenteron starts in:
(a) morula
(b) blastula
(c) early neural
(d) early gastrula
Answer:
(b) blastula
Question 14.
Which of the placenta?
(a) Rabbit
(b) Deer
(c) Sheep
(d) Pig
Answer:
(a) Rabbit

Question 15.
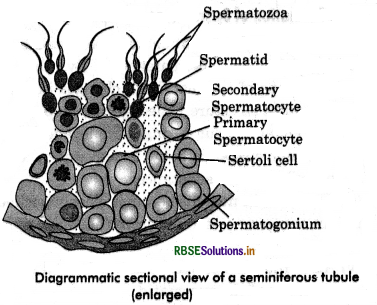
Sertoli cells are located in:
(a) caput epididymis
(b) cauda epididymis
(c) seminiferous tubules
(d) germinal epithelium
Answer:
(c) seminiferous tubules
Question 16.
In 28 day, human ovarian cycle, ovulation occur on:
(a) day 1
(b) day 10
(c) day 14
(d) day 28
Answer:
(c) day 14
Question 17.
Clitoris in mammals is:
(a) homologous to penis
(b) analogous to penis
(c) functional penis in female
(d) non-functional penis in male
Answer:
(a) homologous to penis
Question 18.
Rupturing of follicles and discharge of ova is known as:
(a) copulation
(b) ovulation
(c) opposition
(d) conjugation
Answer:
(b) ovulation
Question 19.
In female mammals, insemination occurs in:
(a) oviduct
(b) vulva
(c) ragina
(d) uterus
Answer:
(c) ragina
Question 20.
How many spermatozoa are produced from one primary spermatocyte?
(a) 6
(b) 4
(c) 2
(d) 8
Answers
(b) 4
Very Short Answer Type Questions
Question 1.
Write the location and function of the sertoli cells in humans:
Answer:
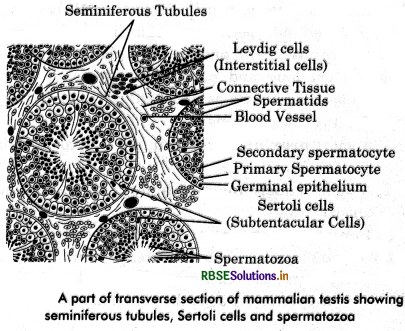
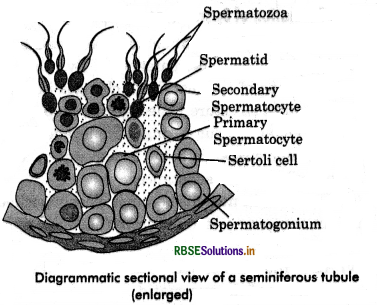
Sertoli cells are present in seminiferous tubules. They provide nutrition to the germ cells are sperms.
Question 2.
Mention the location and the function of Leydig cells in humans:
Answer:
Leydig cells are present in seminiferous tubules. They synthesize and secrete androgens.
Question 3.
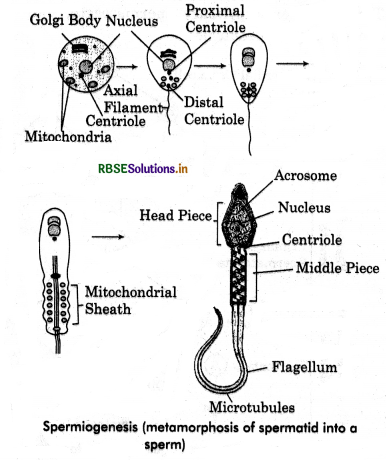
Define spermiogenesis. Where does it occur?
Answer:
Spermiogenesis is the formation of haploid, microscopic and functional spermatozoa (male gametes) from the spermatids. It takes place in the testes (in the male reproductive system).
Question 4.
What is rete testis?
Answer:
Rete testis is a network of the tubules conducting sperm from the seminiferous tubules of the testis to the vasa efferentia.
Question 5.
How does the inguinal hernia develop?
Answer:
the inguinal hernia develops by the tearing of inguinal tissue by any means and may result in the bulging out of a loop of the intestine into the scrotum.
Question 6.
Name the hormone responsible for the descent of the testes into the scrotum. Why does the failure of this process result in sterility?
Answer:
The hormone responsible is testosterone. Failure at the descent of the testes leads to sterility because spermatogenesis does not take place. This is because spermatogenesis requires to a temperature lower than that of the body which is provided by the scrotum.
Question 7.
What is the function of bulbourethral glands?
Answer:
The secretions of the bulbourethral glands help in the lubrication of the penis.
Question 8.
What is the urethral meatus?
Answer:
The urethra originates from the urinary balder and extends through the penis to its external opening called the urethral meatus.

Question 9.
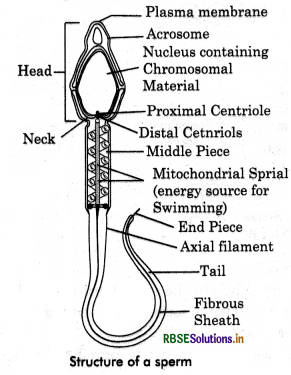
What is acrosome?
Answer:
The acrosome is a cap-like Structure present in the anterior of the head of a sperm.
Question 10.
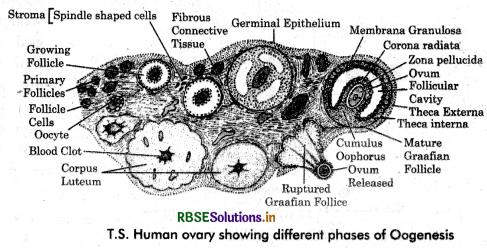
What is corpus leteum?
Answer:
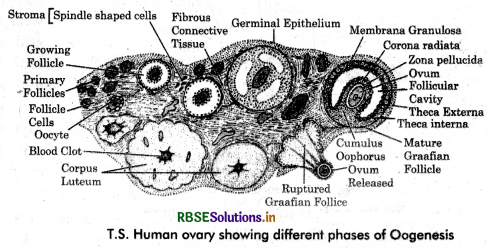
The Corpus leteum is the remaining part of groofian follicle after ovulation in the luteal phase which acts as an endocrine gland.
Question 11.
Where does fertilization normally take place in a human female?
Answer:
Oviduct (Ampullery-isthmus junction of the fallopian tube).
Question 12.
Mention the importance of LH surge during the menstrual cycle.
Answer:
LH surge is essential for the events leading to ovulation.
Question 13.
What is corona radiata?
Answer:
The follicle cells that envelop the egg outside zona pellucid are called corona radiata.
Question 14.
Name the three layers of the uterine wall.
Answer:
- Perimetrium
- Myometrium
- Endometrium.
Question 15.
Name the embryonic stage that gets implanted in the uterine wall of a human female.
Answer:
Blastula.
Question 16.
What is mesovarium?
Answer:
Mesovarium comprises of peritoneum that holds the ovary close to the lateral walls of the pelvic cavity.
Question 17.
Which part in the male reproductive system store sperms? '
Answer:
Epididymis stores sperms.
Question 18.
What is the function of the scrotum?
Answer:
thermoregulation and protection.
Question 19.
Name the sperm lysin which helps in sperm entry into ovum.
Answer:
Hyaluronidase.
Question 20.
Mention the function of trophoblast in the human embryos.
Answer:
Trophoblast obtains nutrition for developing foetus from the placenta.
Question 21.
What is semen?
Answer:
The products of testes (sperms) and prostate gland along with the fluid of seminal vesicles are collectively called semen.
Question 22.
What do you mean by foetal ejection reflix?
Answer:
These are mild uterine contractions induced by the signals for parturition originated from fully developed foetus and placenta.
Question 23.
Why are human testes located outside the abdominal cavity? Name the pouch in which they are present
Answer:
Human testes are located outside the abdominal cavity as it helps in maintaining low temperature (2-2.5°C lower than body temperature) required for spermatogenesis. Testes are located in a pouch called the scrotum.
Question 24.
Write the function of the seminal vesicle.
Answer:
Seminal vesicle produces on alkaline secretion containing prostaglandins, protein and fructose. The high fructose contents provide energy to the spermatozoa. These secretions form 60-70% of the fluid found in the semen.
Question 25.
Mention the function of zona pellucida.
Answer:
During fertilization, a sperm come in contact with the zona pellucida layer of ovum and induces change in the membrane and forms fertilization envelop. It helps block the entry of additional sperms. So, zona pellucida ensures that only one sperm fertilizes an ovum.
Question 26.
State from where do the signals for pacturition originate in human female?
Answer:
Foetal - ejection reflex generated by fully developed foetus and placenta stimulates pituitary to release the hormone oxytocin responsible for parturition.
Question 27.
When do the oogenesis and the spermatogenesis initiate in human females and males, respectively?
Answer:
Oogenesis initiates during foetal or embryonic stage in females where as spermatogenesis in males starts at puberty.

Question 28.
Name the fluid which protects embryo.
Answer:
Amniotic fluid.
Question 29.
Name the term used for metamorphosis of spermatids.
Answer:
Spermiogenesis.
Question 30.
Name the various extra-embryonic membranes.
Answer:
- Chorion
- Amnion
- Yolk sac
- Allantois.
Question 31.
Why is oxytocin called as birth hormone?
Answer:
Oxytocin controls parturition by powerful contractions of myometrium. So, it is called birth hormone.
Question 32.
How many sperms are present in a single ejaculation?
Answer:
About 300-400 million.
Question 33.
What are teratogens?
Answer:
The agents which cause malformations in the developing embryo are called teratogens.
Question 34.
What is capacitation?
Answer:
Activation of sperms within the female tract of mammals is called capacitation, without which fertilization is imposible.
Question 35.
What is the forensic test for rape?
Answer:
Semen contains fructose contributed by seminal vesicles. Fructose is not produced anywhere in the human body. Its presence in the vagina indicates sexual intercourse has occured.
Question 36.
Write down the name of hormone secreted by ovary in the later phase of pregnancy.
Answer:
Relaxin hormone.
Question 37.
Write the importance of colostrum.
Answer:
Colostrum or first milk produced by the mother after birth has high nutrients and antibodies. It protects new born from diseases.
Short Answer Type Questions-I
Question 1.
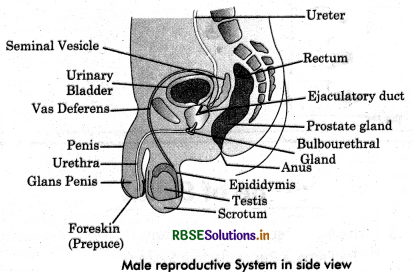
Name the organs which are included in male reproductive system.
Answer:
The organs of male reproductive system:
- Primary reproductive organs: A pair of testes.
- Secondary reproductive organs:
- Accessory ducts: Rete-testis, vasa efferentia, epididymis and vas deferens.
- Accessory glands: Seminal vesicle, prostate and cowper’s gland.
- External genetalio:Penis.

Question 2.
Name the organs which constitute female reproductive system.
Answer:
Organs, that constitute female reproductive system:
- Primary reproductive organs: A pair of ovary.
- Secondary reproductive organs:
- Accessory ducts: Pair of oviducts, uterus, cervix and vagina.
- Accessory glands: Mammary gland.
- External genetalia: Vulva.
Question 3.
Differentiate between gametogenesis in human males and females on the basis of:
(i) time of initiation of the process.
(ii) products formed at the end of the process.
Answer:
|
Process of Gametogenesis |
Males |
Females |
|
Time of initiation of the process. |
Puberty, |
Embryonic development foetal stage. |
|
Products formed at the end of the process. |
Four spermatozoa are produced from are one primary spermatocyte. |
One ovum and two polar bodies produced from one primary oocyte. |
Question 4.
Name the hormones which are secreted by the placenta by the ovary during late pregnancy and also those present only in the pregnant woman.
Answer:
The hormones secreted by placenta are human chorionic gonadotropin (hCG), Human placental Lactogen (hPL), estrogen and progesterone etc. Relaxin is secreted by ovary during late pregnancy.
The hormones which are present only in pregnant woman are : Human chorionic gonadotropin (hCG), Human placental Lactogen (hPL) and relaxin.
Question 5.
Describe the role of corpus luteum.
Answer:
The remnants of graafian follicle, after ovulation forms corpus leteum. It secretes large quantity of the hormone progesterone. This hormone is necessary for the maintenance of endometrium. The later is essential for all the events of pregnancy including the implantation of fertilized egg in the uterus. The corpus leteum starts degenerating if fertilization of egg does riot take place.
Question 6.
Why is there species specificity in fertilization?
Answer:
A chemical substance called ‘fertilizin’ is present on the surface of ovum and similarly the corresponding anti-fertilizin is present on the surface of sperm. The fertilizin and antifertilizin of same species are compatable and of different species incompatible. Therefore, fusion occurs only between compatable gametes. Hence, there is species specificity in fertilization.
Question 7.
Explain what is meant by gametogenesis?
Answer:
The process of the formation of haploid gametes from diploid germ cells in the gonads is called gametogenesis. There are two types of gametes: The spermatozoa and ova. Gametogenesis can be studied under two broad headings : spermatogenesis and oogenesis. Spermatogenesis is the formation of spermatozoa and oogenesis is the formation of ova.
Question 8.
What is menopause?
Answer:
The term menopause literally means “pause in the menses” and refers to the cessation of ovarian activity. The onset is at about the age of 45-50, but varies greatly. Menopause is usually uneventful, but some women suffer from complications such as flushing, excessive bleeding and nervous disorders.
Question 9.
Differentiate between Leydig cells and Sertoli cells.
Answer:
Difference between Leydig cells and Sertoli cells:
|
Leydig Cells (Interstitial Calls) |
Sartoli cells |
|
Leydig cells are present in the connective tissue between the seminiferous tubules.. |
Sertoli cells are present between the cells of germinal epithelium lining seminiferous tubules. |
|
They ate Small groups of pyramidal cells. |
Sertoli cells are elongated and found singly. |
|
These secrete male sex hormone the androgens. |
They provide nurishment to developing spermatozoa. |
Question 10.
Differentiate between vasa efferentia and vasa deferentia.
Answer:
Difference between vasa efferentia and vasa deferentia
|
Vasa Efferentia |
Vasa Defersntia |
|
These arise from rete- testis. |
These arise from cauda epididymis. |
|
They vary from 15-20 in number. |
They are 2 in number. |
|
Their lining bears ciliated cells. |
Their lining has stereocilia. |
|
They carry spermatozoa born the rete-testis to the epididymis. |
They carry spermatozoa from cauda epidilymis to ejaculatory duct. |
Question 11.
Differentiate between Blastulation and Gastrulation.
Answer:
Difference between Blastulation and Gastulation.
|
Characters |
Blastulation |
Gastrulation |
|
Speed of division |
Rapid mitotic division of zygote. |
Slow mitotic divisions |
|
Movements |
Cells do not move. |
Cells masses move from surface of blastula by morphogenetic movement. |
|
Result |
A single-layere hollow blastula is formed. |
A three-layered gastrula, is formed |
Question 12.
What is cleavage? Why is the cleavage in mammals referred as simple holoblastic?
Answer:
The phase of embryogenesis consisting of rapid cell divisions following fertilization is called cleavage. The mitotic divisions during this phase are called cleavage divisions and resulting daughter cells are known as blastomeres. The cleavage in mammals referred as simple haloblastic because cleavage divisions divide the egg completely.
Question 13.
Define the ovulation and fertilization.
Answer:
Ovulation s The process by which an ovum is released from a mature graafian follicle is called ovulation. Fertilization s Fusion of male gamete (sperm) with the female gamete (ovum) is called fertilization.
Question 14.
Why does testing for hCG (Human Chorionic Gonadotropin) work as a pregnancy test early in pregnancy but not late in pregnancy?
Answer:
hCG is secreted by early embryo. It stimulates carpus luteum to secrete progesterone, which helps in maintaining pregnancy. Late during pregnancy (2nd trimester), hCG production drops, corpus leteum disintegrates and secretion of progesterone is taken over by placenta.
Question 15.
What is cumulus oophous and follicular atresia?
Answer:
Cumulus Oophorus: It is the stalk of a heap of granulosa cells that supports the maturing oocyte in a Graafian follicle.
Follicular Atvsia: It refers to the regression, death and disposal of many follicles in the ovary during the reproductive years of the female. These are disposed by the process of phagocytosis.

Question 16.
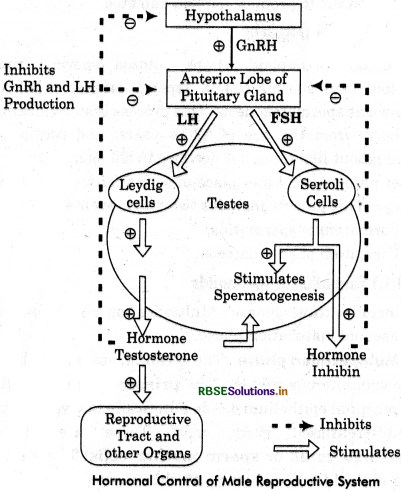
Explain the role of pituitary and sex hormones in the process of spermatogenesis.
Answer:
Hormonal control of spermatogenesis in human males is as follows:
- GnRH is released significantly from the hypothalamus during puberty.
- GnRH stimulates anterior pituitary to secrete gonadotropins i.e., LH and FSH or ICSH.
- LH acts on Leydig cells to stimulate the synthesis and secretion of androgens which then stimulate the process of spermatogenesis.
- Follicle Stimulating Hormone acts on sertoli cells and stimulates them to secrete in hibin which then stimulates the process of spemiogenesis.
Question 17.
Draw a labelled diagram of a human sperm.
Answer:
Question 18.
What happens to corpus luteum in human female if the ovum is (i) fertilized, (ii) not fertilized.
Answer:
- In case of fertilization, the corpus luteum continues secreting progesterone which is required for the maintenance of endometrium during pregnancy.
- In the absence of fertilization, the corpus luteum degenerates and get converted into corpus albicans Deficiency of progesterons causes disintegration of the endometrium leading to menstruation and thus, a new cycle starts.
Question 19.
Why is breastfeeding recommended during the initial period of an infant's growth? Give reasons.
Or
(i) Why is mother’s milk considered very essential for the healthy growth of infants?
(ii) What is the milk called that is produced in the initial days of location.
Answer:
The first milk which comes out from the breasts of mother just after childbirth is known as colostrum. This is a thin, yellowish fluid. It is rich in proteins and energy along with several antibodies (IgA) that provide passive immunity to the newborn.
This immunity helps the neborn to attain resistance to many infections, but it is low in fat and iron content. Hence, breastfeeding during the initial period of growth of infant is highly recommended by the doctors for bringing up a disease free healthy baby.
Question 20.
Differentiate between spermatogenesis and spermiogenesis.
Answer:
Difference between spermiogenesis. spermatogenesis and spermiogenesis
|
Spermatogenesis |
Spermiogenesis |
|
It is the process of formation of sperms from immature germ cells. |
It ' is a process of transformation of a circular spermatid to a motile spermatozoa. |
|
Number of cells increases as each spermatogonium produces four spermatids. |
No change in number of cells as only one spermatid develops |
Question 21.
If the acrosome of sperm is damaged then which process will be affected and how?
Answer:
the acrosome of sperm is filled with a hydrolytic enzymes such as hyaluronidase that help the sperm to penetrate the ovum dissolving zona pellucida. If the acrosome of sperm is damaged the above process can not occur.
Question 22.
Explain the process of spermatogenesis in detail.
Answer:
Spermatogenesis :
The formation of haploid (n) spermatozoa (sperms) from diploid (2n) spermatogonia (sperm mother cells) is known as spermatogenesis. This process is starts during puberty from the age of 13-14 years, and continues throughout life, though it declines in old age. Spermatogenesis takes place in seminiferous tubules of testes.
This process includes two major events:
- Formation of spermatids,
- Formation of spermatozoa.
1. Formation of Spermatids:
It includes three phases: Multiplication phase, growth phase and maturation phase.
1. Multiplication phase:
The germinal epithelium lines the seminiferous tubules. The primordial germ cells of germinal epithelium divide mitotically to give rise the undifferentiated germ cells. These are called spermatogonia or sperm mother cells. These cells are diploid (2a) i.e., having 46 chromosomes in each in human. Spermatogonia or sperm mother cells further divide mitotically to produce a number of spermatogonia,
which are of two types:
spermatogonia type A and spermatogonia type B. Type A spermatogonia serve as stem cell which divide to form additional spermatogonia. Type B spermatogonia are the precursors of sperms. They move towards the lumen of seminiferous tubules and enter a growth phase. These are called spermatocytes. Formation of spermatocytes from spermatogonia is called spermatocytogenesis.
2. Growth Phase: During the growth' phase, the spermatocytes grow in size, accumulate cytoplasm and replicate DNA. These are now known as primary spermatocytes. These are about double the size of spermatogonia.
3. Maturation Phase: Each primary spermatocyte undergoes two successive divisions, called maturation divisions. The first maturation division is reductional or meitotic producing secondary spermatocytes. Each secondary spermatocyte contain haploid (n) or half chromosome number which is 23 in human.
The secondary spermatocyte soon undergo the second maturation division which is like on ordinary mitotic division to .form spermatids. This division is equational, hence each spermatid continues to possess the haploid number of chromosomes. Thus from each primary spermatocyte, four haploid sperrnatides are produced.
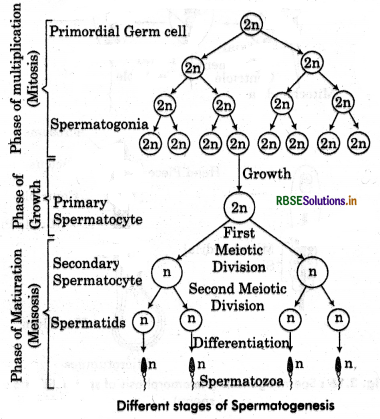
Formation of Spermatozoa or Spermiogenesis:
Transformation of spermatids into spermatozoa is called spermiogenesis or spermateliosis. By this process spherical shape of spermatid cell changes into long and thin thread-like structure, called sperm or spermatozoa. Following changes occur during spermiogenesis :
- The nucleus shrink by losing water, RNA and other accessory substances.
- The DNA in nucleus becomes closely packed.
- An acrosome is formed from the Golgi complex of spermatid.
- Axial filament of sperm tail is formed from distal centriole of the spermatid.
- A mitochondrial spiral around middle piece of sperm is formed from mitochondria. This sheath is known as nebenkern.
- Much of the cytoplasm of spermatid is lost. The remaining cytoplasm forms a sheath around mitochondrial spiral. This sheath is known as Manchetts
A single primary spermatocyte produces four spermatozoa. Sperm cell develops into about two months. The fully formed sperms become free in the cavity of the seminiferous tubules. The process of release of sperms from sertoli cells into the cavity of seminiferous tubule is called spermiation.
From here, they pass via vasa efferentia into the epididymis for temporary storage. During this period, they aquire motility, perhaps under the influence of testosterone hormones.
Hormonal Control of Spermatogenesis:
The process spermatogenesis starts with onset of puberty due to secretion of the hormone, Gonadotropin Releasing Hormone (GnRH) by hypothalamus. This hormone stimulates anterior pituitary to produce two gonadotropic hormones. The Luteinising Hormone (LH) and Follicle Stimulating Hormone (FSH). LH acts on Leyding cells and stimulates synthesis and secretion of androgens such as testosterone.
Testosteron stimulates the process of spermetogenesis. FSH acts on sertoli cells and stimulates them to secrete an Androgen Binding Protein (ABP) and Inhibin. ABP concentrates testosterone in seminiferous tubules. Inhibin suppresses FSH synthesis by anterior pituitary and GnRH synthesis by hypothalamus when there is excess FSH and GnRH. Thus normal release of testosterone is under negative feedback control.
Structure of Spermatozoa (Sperm):
The spermatozoa are microscopic, haploid and motile cells. Sperm remain alive and retain their ability to fertilize an ovum from 24 to 48 hours after having been released in the female genital tract.
A sperm consists of following four parts:
1. Head:
It is enlarged end of sperm. It is flat and oval in human. It is composed of a large posterior nucleus and a small anterior acrosome. Acrosome provides it conical shape of apex and made of Golgi-body. Acrosome and nucleus enclosed in a thin membrane. Spetm nucleus contains densely packed DNA and proteins.,The DNA is present in the aquiescent state. Acrosome is. filled with tissue-dissolving enzymes that help spermatozoan penetrate through the egg membrane and enter the egg cytoplasm.
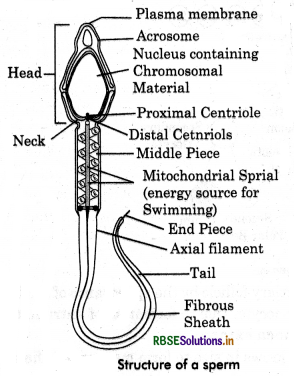
2. Neck:
Neck is very short part and present between the head and middle piece. The neck has two centrioles. The first proximal centriole towards the nucleus which plays a role in the first cleavage of the zygote and second distal centriole gives rise to the axial filament of the sperm.
3. Middle Piece:
The middle piece consists of apical part of the axial filament surrounded by a spiral sheath of numerous mitochondria. The mitochondria provide energy for the movement of the sperm in the female genital tract.
4. Tail:
The tail is several time longer than head. It consists of a central axial filament, thin layer of cytoplasm and" a smooth plasma membrane. The axial filament is formed of nine pairs of longitudinal fibres which extend up to the tip of axial filament. Another set of nine thick, band-like fibres is also present which does not reach the tip of the sperm tail. The free end of tail, without additional fibres, is called end piece.
|
Spermatogenesis |
Spermiogenesis |
|
It is the process of formation of haploid spermatids from diploid germinal cells. |
It is the process of transformation of spermatids |
|
Cytoplasm is added and DNA replicates in this process. |
Golgi complex, cytoplasm and water is lost in this process. |
|
It involves multiplication phase, growth phase and maturation phase. |
It involves only differentiation phase, therefore, it is a part of spermatogenesis. |
|
Four spermatids are produced from a single spermatogonium. |
One spermatozoan is developed from one spermatid. |
Short Answer Type Question-II
Question 1.
What is menstrual cycle? Give a brief account of the phases of menstrual cycle.
Answer:
Menstrual cycle involves cyclic changes in the females reproductive tract culminating in menstruation, that is, flows of cast off uterine lining along with blood and tissue fluid through the vagina.
It consists of three phages:
1. Proliferating Phase:
It lasts for about 14 days. Lining of uterus proliferate and its vascularization increases. A Graafian follicle grows, mature and secretes oestrogen. It ruptures to release its egg after about 14 days.
2. Secretory Phase:
It lasts for about 10 days. The empty Graafian follicle forms in it corpus luteum which secrete progesterone. The lining of uterus undergoes1 further hypertrophy. Endometrial glands of the uterus secrete a nutritive fluid for the foetus.
3. Menstrual (Bleeding) Phase):
It lasts for about 4 days. If fertilization does not occur, the corpus luteum regresses and the lining of uterus breaks down, resulting in menstrual flow. This occurs after about 28 days and continues for 3-5 days.

Question 2.
Write the significance of spermatogenesis and oogenesis.
Answer:
Significance of Spermatogenesis:
- Each primary spermatocyte undergoes two maturation divisions (Meiosis-I and Meiosis-II) and produces four sperms having half number of chromosomes.
- It is necessary to maintain the number of chromosomes constant from generation to generation.
- During Meiosis-I crossing over takes place which brings about variations.
Significance of Oogenesis:
- It produces haploid ovum.
- Polar bodies contain small amount of cytoplasm. It helps to retain adequate amount of cytoplasm in the ovum, which is essential for the development of early embryo.
- During Meiosis-I crossing over takes place which brings about variations.
Question 3.
Describe briefly the structure of human ovum.
Answer:
The human ovum is spherical, non-motile haploid cell. It is almost free of yolk and is said to be alecithal or microlecithal. It has abunded cytoplasm and a centrally located nucleus. The ovum is surrounded by reteline membrane. The ovum shows polarity. Its side, which extrudes polar bodies, is called animal pole. The opposite side is called vegetal pole.
Two additional egg coats enclose the ovum:
inner thin transparent, noncellular zona pellucida and outer cornoa radia'ta. The corona radiata is formed of radially elongated follicular cells, the cells of corona radiata continue to cling to the ovum for sometime after the ovum is released.
Question 4.
What is fertilization in humans? Write about its significance.
Answer:
Fertilization in Human:
It involves the union of a sperm and an ovum to produce a single cell, zygote, from which the body of the offspring is formed.
Significance of Fertilization:
- The sperms contact with the entry into the ovum actiyates the egg. This activation is manifested in egg completing the second meiotic division and many other changes leading to next phase of development i.e., cleavage.
- The fusion of two haploid pronuclei, one from the sperm and other from the ovum restores the diploid condition in the offspring.
- The combination of chromosomes from two different parents produces genetic variations in the offsprings.
Question 5.
What is placenta? Explain briefly. Give its functions.
Answer:
Pregnancy:
Pregnancy is the period of time from conception to the birth of a baby. It is also called gestation period. In pregnancy, the placenta plays a vital role as it provides nutrition to the growing foetus from the mother’s circulatory system. This period is approximately 9 months + 10 days (280 days) in human beings.
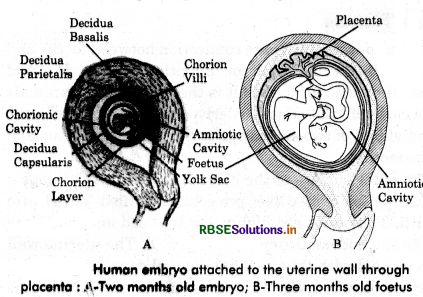
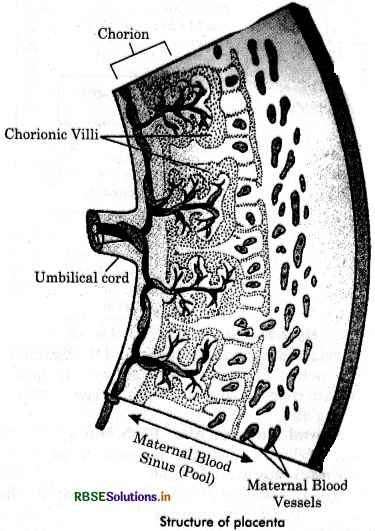
Placenta:
Placenta is the intionate connection between foetus and mother’s uterine wall for nutrition, respiration and excretion etc., for foetus. It is the only organ in animals formed of the tissue derived from two different individual of two successive generations, the foetus and the mother.
The outer surface of the chorion in humans develops a number of finger-like projections, called chorlonic villi. These villi are highly vascularibd and penetrate into the endometriurum wall.
The uterine wall in contact with this a has several depressions called crypts, in which the choriomc viii are embedded. This intimate connection between the foetal membranes and the uterine wall is known as placenta.
Because chorion participates in the formation of placenta, human placenta is called chorionic placenta. The part of the placenta contributed by the foetal membrane is called foetal placenta and that contributed by the mother’s uterine wall aa the maternal placenta or decidua.
Decidua:
Endometriuin of uterine wall, after implantation, becomes modified and called decidua because is separates from endometrium and degenerate after the foetus is delivered (decidun means falling off). Decidua can be differentiated into three regions.
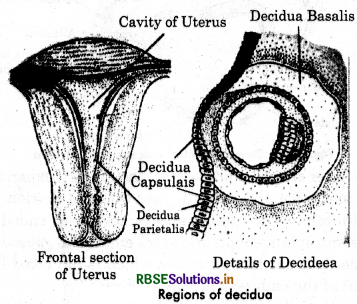
1. Decldua basalls:
It is the part of endometrium between chorion of embryo and the myometrium of uterine wall. Initially it provides glycogen and lipids for the embryo and later on forms maternal part of placenta.
2. Decldua capsulons: It is the region of endometrium between embryo and uterine cavity.
3. Decldua parl.tafls: It is the remaining modified endometrium that lines che rest of the wall of uterus, except the place. where placenta is formed.
Exchange of Mateilals:
In human placenta, foetal blood vessels of chorionie villi bathe directly in the maternal blood due to the erosion of uterine mucosa, connective tissue and endothelial lining of maternal blood vessels. This type of placenta is known as haemochorial or haemoendotheliochorial placenta.
Food and oxygen pass from maternal blood into foetal blood and the excreta from foetus pass into the mother’s blood. The placenta, thus, serves as the nutritive, respiratory and excretory organ for the foetus.
No direct contad between Foetal and Maternal Blood:
The maternal and foetal blood do not mix in the placenta because:
The two may be incompatible.
- he pressure of maternal blood is too high to the foetal blood vessels.
- There mu8t be a check on the passage of harmful materials entering into the foetal blood.
Function of Placenta:
The placenta performs following functions:
1. Nutrition:
All the nutritive substances pass into foetus from mother’s blood through placenta.
2. Respiration:
Placenta helps in exchange of oxygen and carbon dioxide between foetus and mother’sblood and thtts helps in respiration. Oxygen from mother’s blood diffuses into foetus blood and CO2 from foetus blood to mother’s blood.
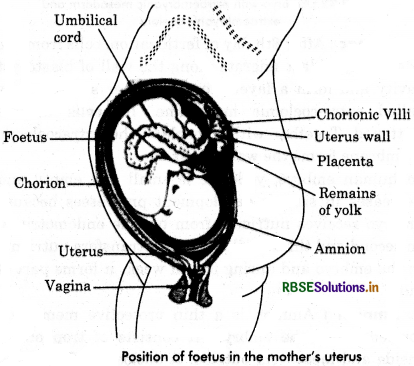
3. Excretion:
Nitrogenous wastes from embryo diffuse into mother’s blood through placenta.
4. Immunity: Antibodies developed in the blood of mother against certain diseases like measles, small pox, diphtheria, scarlet fever etc., are passed from mother’s blood into the foetus. These introduce passive immunity and insusceptibility to these diseases.
5. Storage of Substances : Placenta stores substances such as fat, glycogen and iron and participate in the metabolism of protein.
6. As a Barrier:
Placenta gerves as an efficient barrier and allows those materials to pass into the foetal blood that are necessary. Teratogens are certain agents (viruses or chemicals) or drug that causes abnormal development in developing embryo or foetus. The most well-known synthetic teratogen drug is thalidomide. This drug causes multiple defects in the developing embryo.
7. Endocrin Function:
Placenta secrete following hormones:
(a) Human chorlonlc Gonadotropin (HCG): It is secreted by chorionic cells of placenta soon after implantation of blastocyst. It carries following functions :
- Maintain corpus luteum of pregnancy.
- Stimulates secretion of progesteron and oestrogen by corpus luteum.
- Progesteron maintains endometrial lining of uterus throughout pregnancy, Therefore progesteron ja also called pregnancy hormone.
- Progesteron prevents menstruation.
- It increase s secretion of mucus in cervix forming a protective plurge during pregnancy.
(b) Chorlonic Thyrotropln: Stimulates mother’s thyroid gland to secrete.
(c) Chorlonic Cortlcotropin: Stimulates mother’s adrenal glands for increased secietion of aldosterone. This help mother to retain more sodium and hence more fluid in the body.
(d) Progesteron: Placental progesterone helps in maintaining pregnancy, decreases uterus contractibility and encourages growth of endometrium.
(e) Istrog. Placenta changes adrenal androgen of mother and foetus into oestrogen. This helps in the enlargement of pregnant uterus, growth of brests, growth of external genitalia and in relaxing pelvic ligaments in mother.
(f) Human placental Loctog.n (hPL): This hormone stimulates growth and development of breasts and decreases insulin sensitivity of mother so that mother is not able to utilise own glucose. This makes more glucose available to the foetus.
(g) Relaxirs: This hormone is secreted by both corpus luteum and placenta. This hormone soften connective tissue of pubic symphysis for facilitating easy child birth. Thus increased production of these hormones is essential for supporting foetal growth and metabolic changes in the mother and for maintaining pregnancy.
Question 6.
What is lactation? How is milk production hormonally regulated?
Answer:
Lactation:
The term lactation refers to production of milk. The period after giving birth during which milk is secreted in the breasts of woman. The first secretion from the breast occuring shortly after childbirth is called colostrum. It is rich in calories and protein. Also, it contains antibodies that provide passive immunity for the newborn baby.
Three or four days after deliverly, the breasts begins to secrete milk. Its synthesis is stimulated by the pituitary hormone prolactin. Its release is stimulated by a rise in the level of oxytocin when the baby begins nursing. Milk contains inhibitory peptide. If the breasts are not fully emptied, the peptide accumulates and inhibits milk production. This autocrine action, thus, matches supply with demand.
Question 7.
(i) Draw a labelled diagrammatic view of human male reproductive system.
(ii) Differentiate between vas deferens and vasa efferentia.
Answer:
|
Vasa Efferentia |
Vasa Deferentia |
|
They vary from 15-20 in number. |
They are 2 in number. |
|
These arise from rete testes. |
These arise from cauda epididymis. |
|
Their lining bears ciliated cells. |
Their lining has steriocilia. |
|
They carry spermatozoa from the rete testes to the epididymis. |
These carry spermatozoa from cauda epididymis to ejaculatory duct. |
Question 8.
Explain the events in a normal woman during her menstrual cycle on the following days:
(i) Pituitary hormone levels from 8-12 days.
(ii) Uterine events from 13-15 days.
Answer:
(i) The period of 8-12 d-s after the onset of menstruation is the phase. During this phase, GnRH from hypothalamus stimulates anterior pituitary to release FSH and LH. Former stimulates the ovarian follicles to secrete oestrogen, which in turn stimulates the proliferation of the endometrium of the uterine wall. This causes the endrometrial lining to thicken.
(ii) The uterine events between days 13 to 15 are governed by the high LH and FSH levels. The endometrium is intact due to the effect of these gonadotropin hormones and also prepare itself for pregnancy, if fertilization takes place.
(iii) During 16-23 days, ruptured Graafian follicle gets converted into corpus luteum in the ovary. It starts secreting progesterone which maintains the endo-metrium, necessary for the implantation of fertilised ovum followed by other events of pregnancy.
Question 9.
Explain the events in a normal woman during the menstrual cycle on the following days :
(i) Ovarion events from 13-15 days.
(ii) Ovarion hormones level from 16-23 days.
(iii) Uterine events from 24-29 days.
Answer:
(i) In the ovarian events from 13-15 days, on immature ovum is released from the Graafian follicle. Both LH and FSH attains maximum peak. FSH helps Graafian follicle to attain maturity and LH helps in its rupture. Ovum covered by a number of layers and a yellow fat layer forms corpus luteum. It releases progesterone.
(ii) During mentrual cycle, the period level from 16-23 days is known as luteal phase or secretory phase. The corpus luteum releases large amount of progesterone, which is essential for the maintenance of endometrium.
(iii) Uterine events from 24-29 days are under the influence of progesterone hormone. If influence the maintenance of the endometrium for any pregnancy to occur. In the absence of pregnancy, the corpus lecteum degenerates and endometrium sheds off. It causes the menstrual flow or bleeding.

Question 10.
(i) How many primar / follicles are left in each ovary in a human female of puberty?
(ii) Draw a sectional view of the ovary showing the different follicular stages of a human female in her preovulatory phase of menstrual cycle.
Answer:
(i) A large number of primary follicles degenerate in human female during the period from birth to puberty by the process called follicular atresia. As a result, about 60000-80000 primary follicles are left in each ovary at puberty.
(ii)
Question 11.
Draw a labelled diagram (tic sectional view of a human seminiferous tubule.
Answer:
Question 12.
(i) Explain the process of fertilization in human.
(ii) Name the embryonic stage that gets implanted in huamn females. Explain the process of implantation.
Answer:
(i) The process of a fusion of sperm with an ovum is called fertilization:
1. The motile sperms move through the cervix, enter the uterus and reach the junction of the isthmus and ampulla of the follopian tube.
2. The ovum released from the ovary also reaches the ampullary isthmic junction where fertilization takes place.
3. Fertilization can only occur if the ovum and sperms are transported simultaneously to this junction. This explains why all copulations do not lead to fertilisation and pregnancy.
4. The sperm comes in contact with the zona pellucida of the ovum and releases sperm lysins which induces changes in the egg membrane. It blocks the entry of the other sperms into the egg. Thus, it ensures that only one sperm can fertilize an ovum.
5. The acrosomal secretions help the sperm to enter into the cytoplasm of the ovum through the zona pellucida and the plasma membrane.
6. This induces the completion of meiotic division of the secondary oocyte. The secondary meiotic division results in the formation at a secondary polar body and a haploid ootid (ovum).
7. The haploid nucleus of the sperm and that of ovum fuse together to form diploid zygote.
Implanation: The process of the attachment of the blastocyst to the uterine wall is known as implantation. Though, embryo reaches uterus by the end of 4th day after fertilization, it remains free in the uterine cavity for about 2 days and obtains nutrients from uterine milk. About 8 days after fertilization, blastocyst sinks into the pit formed in the uterine endometrium and gets completely buried.
The lytic enzymes secreted by syncytotrophoblast erode endometrium and enable blastocyst to penetrate uterine wail. The syncytotrophoblast is pushed into finger-like chorionic villi, which interdigitate to establish an intimate contact between blastocyst and endometrium. But the villi from exposed surface of blastocyst are lost. The association of embryo and endometrium is known as implantation. Implantation leads to pregnancy.
(ii) Implantation
The process of the attachment of the blastocyst to the uterine wall is known as implantation. Though, embryo reaches uterus by the end of 4th day after fertilization, it remains free in the uterine cavity for about 2 days and obtains nutrients from uterine milk. About 8 days after fertilization, blastocyst sinks into the pit formed in the uterine endometrium and gets completely buried.
The lytic enzymes secreted by syncytotrophoblast erode endometrium and enable blastocyst to penetrate uterine wail. The syncytiotrophoblast is pushed into finger-like chorionic villi, which interdigitate to establish an intimate contact between blastocyst and endometrium.
But the villi from exposed surface of blastocyst are lost. The association of embryo and endometrium is known as implantation. Implantation leads to pregnancy.
Fotmotlon of Embryonic Disc:
The inner cell mass of blastocyst contamin stem cells, gives rise to all the tissues and organs of the embryo. Immediately after implantation, the cells of inner cell mass get organised into two layers, the epiblast and hypoblast. Both together form a flat embryonic disc.
Hypoblast is primitive endoderm and is formed of a layer of large calumnar cells. Epiblast is the presumptive ectoderm and is formed of two layers of cuboidal cells. A small cavity appears between the two layers of epiblast which develops intc amniotic cavity.
Question 13.
Differentiate between spermatogenesis and oogenesis.
Answer:
|
Spermatogenesis |
Oogenesis |
|
Spermatogenesis occurs in the seminiferous tubules of the testes. |
Oogenesis occurs |
|
It is a continuous process and the growth period is very short. |
It is a discontinuous process' and the growth phase is very long. |
|
It is completed in 74 days in human. |
It completed in a few days to years. |
|
It is completed in testes only. |
It is completed outside the ovary (i.e., fallopian tube). |
|
Each spermatogonium produces four functional spermatozoa. |
Each ooganium producess one functional ovum and three non-functional polar bodies. |
|
Polar bodies are not formed. |
2-3 polar bodies are formed. |
|
All four haploid gametes take part in fertilization. |
Polar nuclei produced during oogenesis do not take part in fertilization. |
Question 14.
Describe the Structure of epididymis.
Answer:
Epididymis:
On the posterolateral side of each testes, there is an elongate, flattened and comma-shaped structure called epididymis. It is formed of a long, about 6 meters, highly convoluted tubes. It is lined with pseudostratified epithelium. The free surface of its columnar cells bears steriocilia. These are actually microvilli that absorb degenerated sperm.
Epididymis shows three regions:
1. Head er Caput Epididymis of Globus Major: It is swollen region present on anterior side of the testes, which receives the sperms from rete testes by 10-12 fine ciliated ductules called vasa efferentia.
2. Body or Corpus Epididymis or Globus Normal: It present on lateral side of testes and stores the sperms for a short period. It is the middle region of epididymis.
3. Tail or Cauda Epididymis or Globus Minor: It lies on caudal side of testes and forms posterior end of epididymis. The semen is concentrated by reabsorption tubules in caput epididymis. Here, sperm mature, become motile and physiologically active to fertilise the egg. From here, sperm pass down to cauda epididymis where they are stored for a while before entering the vas deferens.
The epididymis, by its peristaltic and segmenting contractions, pushes the sperms into the vas deferens sperms (spermatozoa) are produced continuously whether ejaculation takes place or not. If not ejaculated they are reabsorbed.
Functions of Epididymis:
- Epididymis provides passage for sperms from vasa efferentia to vasa deferentia.
- It is involved in storage (for 18-24 hours), nutrition and physiological maturation of the sperms.
- It shows peristaltic and segmenting contractions at intervals to push the sperms away from testes.
Question 15.
What is seminal fluid? Give function of male reproductive system.
Answer:
Seminal Fluid or Semen:
A collection of secretions from the seminal vesicles, prostate gland and cowper’s gland and sperms from testes is known as seminal fluid or semen. It is a milky and viscous mixture having the pH 7.35 to 7.5.
About 3-4 ml semen is ejaculated at one time which contains 200-300 million sperms but out of which atleast 60% sperms must have normal shape and size and at least 40% of them must show vigorous motility for normal fertility. Semen also contains fructose, fibrinogen, proffbrinosin, calcium bicarbonate and mucous.
Functions of Mole Reproductive System:
- Formation of sperms by germinal epithelial cells of . seminiferous tubules by spermatogenesis.
- Production of testosterone hormone and other androgens to maintain it in functional state and develop male secondary characters.
- Transfer of sperm by penis into the vaginal tract of female during copulation
Long Answer Type Questions
Question 1.
(i) Draw a labelled diagram of human male reproductive system.
(ii) Give the structure of testis in brief.
Answer:
(i)
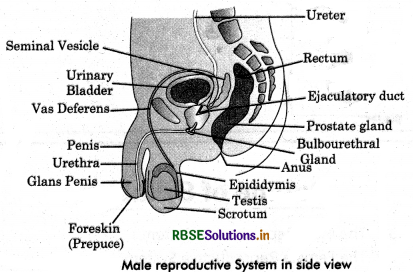
(ii) The testes are primary male reproductive organs. They are soft, smooth, pinkish, oval bodies about 4 - 5 cm long, 2.5 cm wide and 2.4 - 2.5 cm thick. The weight of each testes is about 10 - 12 gm. They are extra - abdominal and held in the scrotal sacs by spermatic cords. In some seasonally breeding mammals, testes descend into the scrotum only in the breeding season as in otter, Bat and Uamba. In Elephant, Whale and Seal, the testes are permanently intra - abdominal.
Structure erf Testes: A testis comprises the following structures:
1. Protective Coverings (Tunicae): Each testis is covered with three layers:
- The outer covering of the testes called tunica vaginalis.
- A fibrous covering inside tunica vaginalis, is called tunica albuginea.
- The tunica vasculosa consists of a network of capillaries supported by loose or delicate connective tissue with abundant blood vessels which lines the tunica albuginea.
2. Testicular Lobules: Each testes has about 200 - 300 compartment called testicular lobules. Each testicular lobule contains 1 - 4 highly convoluted seminiferous tubules, blood vessels and nerves embedded in loose connective tissue. The head of seminiferous tubules converge toward the middle of the posterior surface of the testes and join to form short, straight tubules known as Tubuli recti. These open into a network of wider, irregular tubules called rete testes.
3. Semiferous Tubules: Each seminiferous tubule is thin and coiled structure which is surrounded by a thin membranous sheath made up of connective tissue called tunica propria. Each seminiferous tubule is lined by single layered germinal epithelium. Seminiferous tubules have two types of cells:
- Sporogenic or germ cells and
- Supporting or sertoli cells.
4. Leydig or Interstitial cells: These are present in the connective tissue between the adjacent seminiferous tubules and are small groups of large, polygonal cells. These cells synthesise and secrete testicular hormone called androgens.
5. Rete Testest The end of the semineferous tubules converge toward the middle of the posterior surface of the testes and join to form short straight tubules called tubuli recti. The tubuli recti opens into a network of wider, irregular tubules called rete testis. From the rete testis. 15 - 20 fine convoluted, ductules, the vasa efferentia, pierce the tunica albuginio to enter the head of the epididymis. The vasa efferentia at this places bear cilia to aid in sperm transport.
Functions of Testes: Testes perform:
- The production of sperms by spermatogenesis.
- Secretion of male sex hormones, mainly testosterone by Leydig cells. This hormone promotes development and maintenance of male accessory organs.

Question 2.
(i) Draw a labelled diagram of human female reproductive system.
(ii) Give the structure of human ovary in brief.
Answer:
(i)
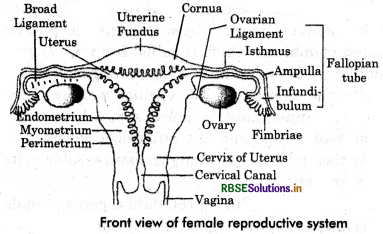
(ii)A pair of ovaries are the primary reproductive organs of a woman. Each ovary is almond - shaped solid, greyish - pink coloured. Measuring about 2 - 4 cm in length, 1.5 cm in width and 1.0 cm in thickness. Each ovary is located near the kidney of its side. It is suspended from the dorsal body wall by a mesentery known as mesovarium, and is attached to the uterus by a double fold of peritoneum, called ovarian ligament. Ovaries are abdominal in position like testes, ovaries have an exocrine function i.e., production of ova and also endocrine function, i.e., secretion of female sex hormones, estrogen and progesterone.
Structure of Ovary:
The ovaries are solid organs and consist of following parts :
1. Ovarian (or Germinal) Epithelium: It is the outermost layer of ovary formed of simple cuboidal cells. Actually, it is modified visceral peritoneum.
2. Tunica albuginea: It is partially differentiated capsule of dense fibrous connective tissue that lies below ovarian epithelium.
3. Stroma: It consists of an outer ovarian cortex and inner ovarian medulla.
- Ovarion Cortex: It is more dense outer part of ovary, which contains young and mature follicles. It also contains a large mass of yellow cells known as corpus luteum in the antrum of ruptured Graafian Follicle after the release of its ovum. Corpus luteum secretes the hormone progesterone during pregnancy, and the hormone relaxin towards the end of pregnancy. The ovarian cortex also has a white body called corpus albicans, which represents the degenerating corpus luteum.
- Ovarian Medula: It contains many rounded or oval structures called ovarian follicles in various stages of development. Each Follicle contains a large ovum sorrounded by many layer of follicle cells. The follicle cells of a maturing follicle secrete estrogen hormone into the blood.
Question 3.
(i) Give name and functions of accessory reproductive glands of human male.
(ii) Give name and function of accessory reproductive glands of human female.
Answer:
(i) The accessory sex glands include a pair of seminal vesicles, prostate gland and a pair of cowpers’ gland or bulbourethral glands.
1. Seminal Vesicle: These are one pair of elongated, coiled sacs about 4 cm long. These are situated between the posterior surface of urinary bladder and the rectum on both sides. Mucous membrane of seminal vesicles contains many goblet cells. Seminal vesicles secrete a yellow mucous like alkaline fluid which is released during ejaculation as a result of contraction of these vesicle and forms a larger portion of the semen. This fluid contains prostaglandins, fructose and seminogelin protein. The alkaline semen neutralizes the acidity of the vagina of the female at the time of sexual intercourse. Fructose is utilised by sperms as a source of energy, prostaglandins induce contraction in vaginal muscles which maintains the activity of sperms. Seminogelin protein induces coagulation of semen to make it more dense.
2. Prostate Gland: It is cone - shaped structure situated around the basal part of urethra below the urinary bladder. It is partially glandular and partially fibro - muscular. It is divided into many lobes and each lobe opens into the urethra through a separate tubule. During ejaculation prostate gland secretes a white and slightly acidic fluid which constitutes about one fourth part of the semen. This secretion contains citrate, phosphate and a variety of proteolytic enzymes like hyaluronidase lysozyme etc. These substances inhibit the overcoagulation of semen so that the activity of sperms does not get hampered. In males, the size of the prostate gland increases after the age of 45 to 50 years as a result of benign hypertrophy so that the urethra is pressed and urination is hindered. Then the gland is surgically cut and removed. Sometimes the gland may suffer from progress atrophy instead of benign hypertrophy.
3. Bulbourethral Glands: These are also called cowper’s gland. These glands are of the size of a pea seed and secrete an alkaline fluid which coats urethra before the release of sperms to neutralise acids of uterine. These glands also secrete mucous which lubricates the end of the penis and lining of urethra.
(ii) Glands Related with Female Reproductive System:
1.Bertholin Glands or Vestibular Glands: A pair of Bertholin glands are present one on each side of the vaginal orifice. These glands correspond to the Cowper’s gland of the male. They are small rounded bodies. Their ducts open just outside the hymen into the vestibule. These glands secrete a clear, viscous fluid under sexual excitement. This fluid serves as a lubricant during copulation.
2. Perineal Glands: One pair of perineal glands are situated just behind Bertholin glands. These produce a specific odorous secretion, which produces sexual excitement.
3. Rectal Glands s One pair of yellow coloured rectal glands is located on both side of rectum. Its secretions produce specific odorous secretion.
Function of Fomole Reproductive System:
- Production of ova from the germinal epithelial cells of ovary. Only one ovum is produced at an interval of 28 days.
- Fertilization of ovum by sperm in the fallopian tube.
- Implantation of fertilized ovum in the uterus.
- Nourishment and protection to the growing foetus.
- Post - natal nourishment of the body.
- Antibodies in the milk provide protection to the infant from infection.
Question 4.
Write short notes on the following:
(i) Sertoli cells
(ii) Leydig cells
(iii) Urethra
(iv) Rete testin.
Answer:
(i) Sertoli cells:
Supporting or Sertoli cells: Some cells of germinal epithelium in seminiferous tubules are pyramidal in shape, called sertoli cells
Functions of Sertoli Cells:
- Sertoli cells provide nutrition to developing sperms,
- These also provide mechanical support to the developing sperms during spermatogenesis.
- These secrete Androgen Binding Protein (ABP) that concentrates testosterone in the seminiferous tubules.
- These also secrete another protein hormone called inhibin which suppresses FSH synthesis.
- These cells disintegrate the excess amount of cytoplasm of spermatids.
(ii) Leydig cells
Leydig or Interstitial cells: These are present in the connective tissue between the adjacent seminiferous tubules and are small groups of large, polygonal cells. These cells synthesise and secrete testicular hormone called androgens.
(iii) Urethra
Urethra arises from urinary bladder and joins the ejaculatory duct to form urinogenital canal. It carries urine as well as sperm and secretions of seminal vesicles, prostate gland and cowper’s gland. Urethra is about 30 cm long and passes through penis to its external opening known as urethral meatus. Urethra has following three regions:
- A short proximal prostotic part surrounded by prostate gland.
- A short middle membranous Urethra without any covering.
- Penial part, that passes through the penis.
(iv) Rete testin.
Rete Testest The end of the semineferous tubules converge toward the middle of the posterior surface of the testes and join to form short straight tubules called tubuli recti. The tubuli recti opens into a network of wider, irregular tubules called rete testis. From the rete testis. 15 - 20 fine convoluted, ductules, the vasa efferentia, pierce the tunica albuginio to enter the head of the epididymis. The vasa efferentia at this places bear cilia to aid in sperm transport.
Functions of Testes: Testes perform:
- The production of sperms by spermatogenesis.
- Secretion of male sex hormones, mainly testosterone by Leydig cells. This hormone promotes development and maintenance of male accessory organs.

Question 5.
Write short notes on the following:
(i) Uterus
(ii) Cervix
(iii) Mammary glands.
Answer:
(i) Uterus:
Uterus is a hollow and inverted pear-shaped structure having thick muscular wall. It is located in the pelvic cavity between the urinary bladder and rectum. It is attached to the body wall by a double fold of ligaments, the mesometrium. Uterus is about 8 cm long, 5 cm wide and 2 cm thick.
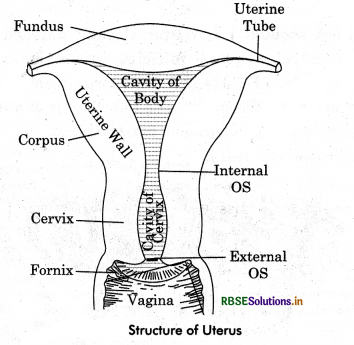
(ii) Cervix :
It is the lower narrow part that projects into the vagina.The cervix communicates with the body of the uterus by an aperture the internal Os, and with the vagina below by an opening, the external Os. The cavity of cervix between the internal Os and external Os is called cervical canal. It is about 2.5 cm long. The glands of the cervical canal secrete a protective mucous plug during pregnancy.
(iii) Mammary glands:
The breast are rounded protuberances situated over the pectoral muscles on the front of wall of the thorax. These are two in number. The mammary glands are milk- producing modified sweat glands which occur in both the breasts, breasts have pads of fatty tissue. They are also present in the male but only in rudimentry form. In the female, they are undeveloped until puberty. These enlarge considerably in the adult female. Each breast has near its middle a nipple surrounded by a circular, pigmented (deep pink to brown or blackish) area called areola. The mammary glands are compound saccular glands. The connective tissue supports the mammary glands and the adipose tissue covers them. The mammary glands open on the nipples by lactiferous ducts. Just under the nipples, the lactiferous ducts widen to form lactiferous sinuses to store milk during lactation.
Question 6.
Describe the roles of pituitary and ovarian hormones during the menstrual cycle in a human female.
(i) Explain the ovarian and uterine events that occur during a menstrual cycle in a human female under the influence of pituitary and ovarian hormone, respectively.
Answer:
Menstruation means the discharge of blood and of fragments of endometrium from the vagina at intervals of 28 days in women of childbearing age. Menstruation cycle comprises of four phases, that are regulated by pituitary hormones (LH and FSH) as well as ovarian hormones (oestrogen and progestrone) that effects ovaries and uterus, respectively. The events occuring in a menstrual cycle are as follows:
|
Phase |
Effects of Hormones |
|
1. Menstrual Phase (from 3rd - 5th day in a 28 day cycle). |
1. Initiated by reduced secretion of Luteinising hormone (LH), progesterone, and oestrogen. The endometrium of uterus breaks down and blood along with unfertilized ovum constitute menstrual flow. |
|
2. Follicular Phase (from 6th - 13th day in a cycle). |
2. The follicle stimulating Hormone (FSH) secreted by anterior pituitary stimulates ovarian follicle to secrete oestrogens. These stimulate proliferation of uterine wall as a result of which endometrium gets thickened. |
|
3. Ovulatory Phase (14th day in 28 day cycle). |
3. LH and FSH from pituitary reach the highest level in middle of the cycle. Rapid secretion of LH causes ovulation thus, inducing the rupture of Graafian follicle to release secondary oocyte and a polar body. |
|
4. Luteal or Secretory Phase (From 15th - 28th day in a 28 days cycle). |
4. LH from pituitary, stimulates the remaining cells of ovarian follicle to develop in to corpus luteum. It secretes large amount of progesterone which maintains endometrial thickening for implentation of blastoeyst. In the absence of fertilization, the harmone levels are reduced (LH and progesterone) and endomerium disintegrates leading to onset of another menstrual cycle. |
Question 7.
During the reproductive cycle of a human female when, where and how does placenta develop? What is the function of placenta during pregnancy and embryo development?
Answer:
Placenta is the intionate connection between foetus and mother’s uterine wall for nutrition, respiration and excretion etc., for foetus. It is the only organ in animals formed of the tissue derived from two different individual of two successive generations, the foetus and the mother. The outer surface of the chorion in humans develops a number of finger-like projections, called chorionic villi.
These villi are highly vascularized and penetrate into the endometrium of the wall. This intimate connection between the foetal membranes and the uterine wall is known as placenta. Because chorion participates in the formation of placenta, human placenta is called chorionic placenta. The part of the placenta contributed by the foetal membrane is called foetal placenta and that contributed by the mother’s uterine wall as the maternal placenta or decidua.
Decidua: Endometrium of uterine wall, after implantation, becomes modified and called decidua because is separates from endometrium and degenerate after the foetus is delivered (decidua means falling off). Decidua can be differentiated into three regions.
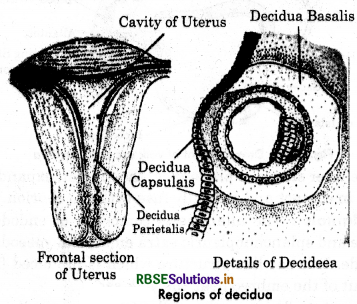
- Decidua basalis
- Decidua capsularis
- Decidua parieralis
Exchange of Materials: In human placenta, foetal blood vessels of chorionic villi bathe directly in the maternal blood due to the erosion of uterine mucosa, connective tissue and endothelial lining of maternal blood vessels. This type of placenta is known as haemochorial or haemoendotheliochorial placenta. Food and oxygen pass from maternal blood into foetal blood and the excreta from foetus pass into the mother’s blood. The placenta, thus, serves as the nutritive, respiratory and excretory organ for the foetus.
No direct contact between Foetal and Maternal Blood:
The maternal and foetal blood do not mix in the placenta because :
- The two may be incompatible.
- The pressure of maternal blood is too high to the foetal blood vessels.
- There must be a check on the passage of harmful materials entering into the foetal blood.
Question 8.
Explain the process of fertilization and implantation in human.
Or
(i) Briefly explain the events of fertilization and implentation in an adult human female.
(ii) Comment on the role of placenta as an endocrine gland.
Answer:
(i) The process of a fusion of sperm with an ovum is called fertilization:
1. The motile sperms move through the cervix, enter the uterus and reach the junction of the isthmus and ampulla of the follopian tube.
2. The ovum released from the ovary also reaches the ampullary isthmic junction where fertilization takes place.
3. Fertilization can only occur if the ovum and sperms are transported simultaneously to this junction. This explains why all copulations do not lead to fertilisation and pregnancy.
4. The sperm comes in contact with the zona pellucida of the ovum and releases sperm lysins which induces changes in the egg membrane. It blocks the entry of the other sperms into the egg. Thus, it ensures that only one sperm can fertilize an ovum.
5. The acrosomal secretions help the sperm to enter into the cytoplasm of the ovum through the zona pellucida and the plasma membrane.
6. This induces the completion of meiotic division of the secondary oocyte. The secondary meiotic division results in the formation at a secondary polar body and a haploid ootid (ovum).
7. The haploid nucleus of the sperm and that of ovum fuse together to form diploid zygote.
Implanation: The process of the attachment of the blastocyst to the uterine wall is known as implantation. Though, embryo reaches uterus by the end of 4th day after fertilization, it remains free in the uterine cavity for about 2 days and obtains nutrients from uterine milk. About 8 days after fertilization, blastocyst sinks into the pit formed in the uterine endometrium and gets completely buried.
The lytic enzymes secreted by syncytotrophoblast erode endometrium and enable blastocyst to penetrate uterine wail. The syncytotrophoblast is pushed into finger-like chorionic villi, which interdigitate to establish an intimate contact between blastocyst and endometrium. But the villi from exposed surface of blastocyst are lost. The association of embryo and endometrium is known as implantation. Implantation leads to pregnancy.
(ii) Placenta: Placenta is the intionate connection between foetus and mother’s uterine wall for nutrition, respiration and excretion etc., for foetus. It is the only organ in animals formed of the tissue derived from two different individual of two successive generations, the foetus and the mother.
The outer surface of the chorion in humans develops a number of finger-like projections, called chorionic villi. These villi are highly vascularized and penetrate into the endometrium of the wall. This intimate connection between the foetal membranes and the uterine wall is known as placenta. Because chorion participates in the formation of placenta, human placenta is called chorionic placenta. The part of the placenta contributed by the foetal membrane is called foetal placenta and that contributed by the mother’s uterine wall as the maternal placenta or decidua.
Decidua: Endometrium of uterine wall, after implantation, becomes modified and called decidua because is separates from endometrium and degenerate after the foetus is delivered (decidua means falling off). Decidua can be differentiated into three regions.
- Decidua basalis
- Decidua capsularis
- Decidua parieralis
Exchange of Materials: In human placenta, foetal blood vessels of chorionic villi bathe directly in the maternal blood due to the erosion of uterine mucosa, connective tissue and endothelial lining of maternal blood vessels. This type of placenta is known as haemochorial or haemoendotheliochorial placenta. Food and oxygen pass from maternal blood into foetal blood and the excreta from foetus pass into the mother’s blood. The placenta, thus, serves as the nutritive, respiratory and excretory organ for the foetus.
No direct contact between Foetal and Maternal Blood:
The maternal and foetal blood do not mix in the placenta because :
- The two may be incompatible.
- The pressure of maternal blood is too high to the foetal blood vessels.
- There must be a check on the passage of harmful materials entering into the foetal blood.

Question 9.
(i) Explain the following phases in the menstrual cycle of a human female:
(a) Menstrual phase
(b) Follicular phase
(c) Luteal Phase.
(ii) A proper understanding of menstrual cycle can help immensely in family planning. Do you agree with the statement? Provide reasons for your answer.
Answer:
(i)
(a) Menstrual Phase: It marks the beginning of menstrual cycle. It is characterised by menstrual flow and lasts 3 to 5 days. The menstrual flow takes place due to breakdown of endometrial lining of uterus and its blood vessels. Therefore, unfertilized ovum alongwith ruptured uterine epithelium, about 50-100 ml of blood and some mucous is discharged out through the vaginal orifice and is called menstrual flow (or monthly bleeding).
Menstruation occurs only if the released ovum is not fertilized. Failure of menstruation indicates pregnancy but it may also be disturbed due to mental and physical stress or poor health etc.
(b) Follicular Phase: It is also called post-menstrual or pre-ovulatory phase which extends from 6th day to 13th day of the menstrual cycle. It is characterised by following events :
- Primary follicle in the ovary grows into a fully mature Graafian follicle.
- Endometrium of uterine wall regenerates and ruptured blood vessels are repaired.
- The endometrium and its uterine glands grow by tissue proliferation. Hence, follicular phase is also known as proliferative phase.
During follicular phase, the changes are controlled by estrogens secreted by ovary and follicle cells of maturing Graafian follicle. The level of estrogens is maximum during follicular phase and it is maintained by FSH of anterior pituitary. By the end of this phase, endometrium of uterus becomes 2-3 mm thick and the endometrial glands become coiled and cork screw-shaped. The arterioles in uterus wall also grow longer and branched, making the endometrium highly vascular.
(c) Luteal or Secretory Phase: The period that follows ovulation is called luteal phase. During this period cells of suptured Graafian follicle grow in size and form yellow coloured corpus luteum. It grows for about 7 days and secretes progesteron hormone. The level of this hormone is controlled by LH. In this period, uterine endometrium further proliferates and is ready for implantation. In case ovum is not fertilized, corpus luteum degenerates into a white mass called corpus albicans. This lowers the level of progesterone in blood.
When ovum is fertilized, progesteron further prepares the uterus for anticipated pregnancy. The uterine endometrium thickens further up to 4-5 mm. Uterine glands increase and secrete uterine fluid for nourishing the dividing ovum. The uterus is ready for implantation of the embryo. Progesteron also inhibits further follicular maturation. The progesteron level is the highest during luteal phase, hence called progesteron phase. The duration of this phase is pretty constant lasting usually 14 days i.e., from 15th to 28th day of the cycle.
(ii) Yes, a proper understanding of menstrual cycle can help in family planning as this information can be used to avoid the meeting of sperms and ovum. This is known as periodic abstinence or rhythm method of birth control, i.e., temporary avoidance of sex. In this method, a couple can avoid or abstain the coitus from day 10 to 17 of the menstrual cycle because ovulation occurs during this period. The chances of fertilization are very high during this period.
Question 10.
(i) Explain the process of spermotogenesis in humans.
(ii) Draw a human sperm and label acrosome and middle piece. Mention their functions.
Answer:
(i) Formation of haploid (n) spermotozoa (sperms) from diploid (2n) spermatogonia (sperm mother cells) is known as spermatogenesis. This process is starts during puberty from the age of 13-14 years, and continues throughout life, though it declines in old age. Spermatogenesis takes place in seminiferous tubules of testes. This process includes two major events :
- Formation of spermatids,
- Formation of spermatozoa.
Formation of Spermatids:
It includes three phases: Multiplication phase, growth phase and maturation phase.
1. Multiplication phase: The germinal epithelium lines the seminiferous tubules. The primordial germ cells of germinal epithelium divide mitotically to give rise the undifferentiated germ cells. These are called spermatogonia or sperm mother cells. These cells are diploid (2a) i.e., having 46 chromosomes in each in human. Spermatogonia or sperm mother cells further divide mitotically to produce a number of spermatogonia, which are of two types : spermatogonia type A and spermatogonia type B. Type A spermatogonia serve as stem cell which divide to form additional spermatogonia. Type B spermatogonia are the precursors of sperms. They move towards the lumen of seminiferous tubules and enter a growth phase. These are called spermatocytes. Formation of spermatocytes from spermatogonia is called spermatocytogenesis.
2. Growth Phase: During the growth' phase, the spermatocytes grow in size, accumulate cytoplasm and replicate DNA. These are now known as primary spermatocytes. These are about double the size of spermatogonia.
3. Maturation Phase: Each primary spermatocyte undergoes two successive divisions, called maturation divisions. The first maturation division is reductional or meitotic producing secondary spermatocytes. Each secondary spermatocyte contain haploid (n) or half chromosome number which is 23 in human. The secondary spermatocyte soon undergo the second maturation division which is like on ordinary mitotic division to .form spermatids. This division is equational, hence each spermatid continues to possess the haploid number of chromosomes.
Thus from each primary spermatocyte, four haploid spermatids are produced.
Formation of spermatozoa:
Transformation of spermatids into spermatozoa is called spermiogenesis or spermateliosis. By this process spherical shape of spermatid cell changes into long and thin thread-like structure, called sperm or spermatozoa. Following changes occur during spermiogenesis :
- The nucleus shrink by losing water, RNA and other accessory substances.
- The DNA in nucleus becomes closely packed.
- An acrosome is formed from the Golgi complex of spermatid.
- Axial filament of sperm tail is formed from distal centriole of the spermatid.
- A mitochondrial spiral around middle piece of sperm is formed from mitochondria. This sheath is known as nebenkern.
- Much of the cytoplasm of spermatid is lost. The remaining cytoplasm forms a sheath around mitochondrial spiral. This sheath is known as Manchetts.
A single primary spermatocyte produces four spermatozoa. Sperm cell develops into about two months. The fully formed sperms become free in the cavity of the seminiferous tubules. The process of release of sperms from sertoli cells into the cavity of seminiferous tubule is called spermiation. From here, they pass via vasa efferentia into the epididymis for temporary storage. During this period, they aquire motility, perhaps under the influence of testosterone hormones.
(ii)

Question 11.
Explain the menstrual phase in a human female. State the level of ovarian and pituitary hormones during this phase.
(ii) Why is pollicular phase in the menstrual cycle also referred as proliferative phase? Explain.
(iii) Explain the events that occur in a Graafian follicle at the time of ovulation and thereafter.
(iv) Draw a Graafian follicle and label antrun and secondary oocyte. [Delhi 2016]
Answer:
(i) Menstruation means the discharge of blood and of fragments of endometrium from the vagina at intervals of 28 days in women of childbearing age. Menstruation cycle comprises of four phases, that are regulated by pituitary hormones (LH and FSH) as well as ovarian hormones (oestrogen and progestrone) that effects ovaries and uterus, respectively. The events occuring in a menstrual cycle are as follows:
|
Phase |
Effects of Hormones |
|
1. Menstrual Phase (from 3rd - 5th day in a 28 day cycle). |
1. Initiated by reduced secretion of Luteinising hormone (LH), progesterone, and oestrogen. The endometrium of uterus breaks down and blood along with unfertilized ovum constitute menstrual flow. |
|
2. Follicular Phase (from 6th - 13th day in a cycle). |
2. The follicle stimulating Hormone (FSH) secreted by anterior pituitary stimulates ovarian follicle to secrete oestrogens. These stimulate proliferation of uterine wall as a result of which endometrium gets thickened. |
|
3. Ovulatory Phase (14th day in 28 day cycle). |
3. LH and FSH from pituitary reach the highest level in middle of the cycle. Rapid secretion of LH causes ovulation thus, inducing the rupture of Graafian follicle to release secondary oocyte and a polar body. |
|
4. Luteal or Secretory Phase (From 15th - 28th day in a 28 days cycle). |
4. LH from pituitary, stimulates the remaining cells of ovarian follicle to develop in to corpus luteum. It secretes large amount of progesterone which maintains endometrial thickening for implentation of blastoeyst. In the absence of fertilization, the harmone levels are reduced (LH and progesterone) and endomerium disintegrates leading to onset of another menstrual cycle. |
(ii) In follichlar phase primary follicles in the ovary grow under the influence of FSH. It starts from 6th day and ends on 13th and 14th day of 28 day cycle. FSH also stimulates, the ovarian follicles to secrete oestrogen which in turn stimulates endometrium to proliferate, so that it becomes thicker and highly vascularised. Thus it is also called proliferative phase at menstrual cycle.
(iii) Graafian Follicle at Ovulation: At the time of ovulation following events occur:
- LH and FSH reach at their peak levels (about 14th - 16th day of cycle).
- High level of LH induces Graafian follicle to rupture and release the secondary oocyte from it.
- After ovulation, the remaining cells of Graafian follicle are stimulated by LH to develop corpus luteum.
(iv) Diagrammatic sectional view of Graafian follicle See fig 3.2 in text.
Question 12.
(i) Arrange the following hormones in the sequence oif their secretion in a pregnant woman.
hCG, LH, FSH, Relaxin.
(ii) Mention their source and the function they perform.
Answer:
(i) The sequence of secretion of the given hormones in a pregnant woman is :
FSH → LH → hCG → Relaxin
(ii)
|
Hormone |
Source |
Function |
|
FSH |
Anterior |
Stimulates the growth of ovarian follicles in ovary. |
|
LH |
Anterior lobe at pituitary |
It triggers ovulation. |
|
hCG |
Placenta |
It otimulates the corpus luteum to secrete progesterone. |
|
Relaxin |
Placenta |
If facilitates porturition by softening the connective tissue of pubis symphysis. |
Question 13.
(i) Explain menstrual cycle in human female
(ii) How can the scientific understanding of the menstrual cycle of human females help as a centraceptive measure?
Answer:
(I) The reproductive cycle in female primates (Monkeys, apes and humans) is known as menstrual cycle. In a woman, sexual cycle begins when a girl attains puberty. The first menstruation in a girl is called menarche. Menstruation is repeated at an average interval of 28 days. In the middle of each cycle, one ovum is released from either of the two ovaries. The cycle of events starting from one menstruation to the next is called menstrual cycle. The menstrual cycle consists of four phases.
1.Menstrual Phase: It marks the beginning of menstrual cycle. It is characterised by menstrual flow and lasts 3 to 5 days. The menstrual flow takes place due to breakdown of endometrial lining of uterus and its blood vessels. Therefore, unfertilized ovum alongwith ruptured uterine epithelium, about 50-100 ml of blood and some mucous is discharged out through the vaginal orifice and is called menstrual flow (or monthly bleeding).
Menstruation occurs only if the released ovum is not fertilized. Failure of menstruation indicates pregnancy but it may also be disturbed due to mental and physical stress or poor health etc.
2. Follicular Phase: It is also called post-menstrual or pre-ovulatory phase which extends from 6th day to 13th day of the menstrual cycle. It is characterised by following events :
- Primary follicle in the ovary grows into a fully mature Graafian follicle.
- Endometrium of uterine wall regenerates and ruptured blood vessels are repaired.
- The endometrium and its uterine glands grow by tissue proliferation. Hence, follicular phase is also known as proliferative phase.
During follicular phase, the changes are controlled by estrogens secreted by ovary and follicle cells of maturing Graafian follicle. The level of estrogens is maximum during follicular phase and it is maintained by FSH of anterior pituitary. By the end of this phase, endometrium of uterus becomes 2-3 mm thick and the endometrial glands become coiled and cork screw-shaped. The arterioles in uterus wall also grow longer and branched, making the endometrium highly vascular.
3. Ovulatory Phase : It involves the ovulation from the Graafian follicle of ovary. LH and FSH level peak on the 14th day of menstrual cycle. The maximum level of LH during mid cycle (i.eon 14th day) is called LH surge. It induces rupture of graafian follicle and release of ovum. There is no more change in uterine endometrium during this phase.
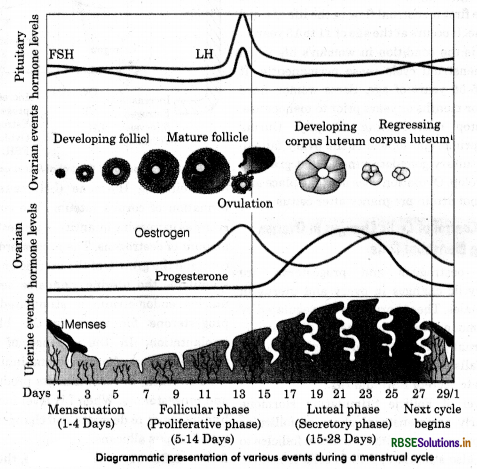
Luteal or Secretory Phase: The period that follows ovulation is called luteal phase. During this period cells of suptured Graafian follicle grow in size and form yellow coloured corpus luteum. It grows for about 7 days and secretes progesteron hormone. The level of this hormone is controlled by LH. In this period, uterine endometrium further proliferates and is ready for implantation. In case ovum is not fertilized, corpus luteum degenerates into a white mass called corpus albicans. This lowers the level of progesterone in blood.
When ovum is fertilized, progesteron further prepares the uterus for anticipated pregnancy. The uterine endometrium thickens further up to 4-5 mm. Uterine glands increase and secrete uterine fluid for nourishing the dividing ovum. The uterus is ready for implantation of the embryo. Progesteron also inhibits further follicular maturation. The progesteron level is the highest during luteal phase, hence called progesteron phase. The duration of this phase is pretty constant lasting usually 14 days i.e., from 15th to 28th day of the cycle.
(ii) Yes, a proper understanding of menstrual cycle can help in family planning as this information can be used to avoid the meeting of sperms and ovum. This is known as periodic abstinence or rhythm method of birth control, i.e., temporary avoidance of sex. In this method, a couple can avoid or abstain the coitus from day 10 to 17 of the menstrual cycle because ovulation occurs during this period. The chances of fertilization are very high during this period.

Question 14.
Given below is the diagram of a human ovum surrounded by a few sperms. Study the diagram and answer the following questions:

(i) Which one of the sperm would reach the ovum earlier.
(ii) Identity ‘D’ and ‘E' Mention the rqle of ‘E’.
(iii) Mention what helps the entry of sperm into the ovum and write the changes occuring in the ovum during the process.
(iv) Name the specific region in the female reproductive system where the event represented in the diagram takes place.
Answer:
(i) Sperm ‘A’ would reach the ovum earlier.
(ii) D. Corona radiate, E. Zona pellucide. During fertilization, a sperm comes in contact with zona pellucida layer of the ovum and induces changes in the membrane that block the entry of additional sperms. Hence E helps to prevent polyspermy.
(iii) The hydrolytic secretion of acrosome help the sperm to enter into cytoplasm of the ovum through the zona pellucida and the plasma membrane. This induces the completion of the meiotic division of the secondary oocyte.
(iv) These events take place in the ampullary - isthmic junction at the fallopian tube.
Question 15.
Write short notes on parturition and lactation.
Answer:
The process of expelling the full term foetus from mother’s uterus at the end of gestation is called parturition. The duration of pregnancy in human beings is about 9 months ± 7 days approximately which is known as gestation period. The gestation is completed in about 280 days from the start at mother’s last menturation.
Machanism of Parturition : The foetus signals that it is mature by secreting certain hormones. These hormones diffuse through placenta into mother’s blood which cause secretion of oxytocin. Oxytocin stimulates uterine contractions. This provides force to expel the baby from the uterus, causing birth. Oxytocin also stimulates the placenta to secrete prostaglandins. They stimulate more contractions of uterus. Uterin contractions by positive feedback induce continuation of oxytocin and prostaglandins production.
The contractions are induced by placental and foetal hormones together. They are :
- Estrogen: The level of estrogens in female increases many folds, totwards the end of gestation. Its high level counteracts effect of progesteron that maintain pregnancy, makes uterine muscules sensitive to oxytocin and stimulates foetal onterior pituitary to senete ACTH (Adrenocarticotropic Hormone).
- Oxytocin: It is also known as birth hormone because it stimulates contraction of uterine muscles. The release of oxytocin by posterior pituitary of mother, is induced by stimuli from uterine contractions.
- Relaxin: It is secreted by placenta. It increases flexibility, of pubic symphysis and dilutes cervix, during labour.
- Prostaglandins: Estrogen stimulates placenta to release prostaglandins which in turn induce production of enzymes for the digestion of collagen fibres in cervix.
- Corticotropin-Releasing Hormone: It is secreted by placenta towards the end of gestation to establish time of birth.
Labour Pain
The forceful muscular, contraction of the uterine wall leading to parturition is known as labour. The term is appropriate as it is a period of act at the expense of considerable energy. About two weeks before birth, the fortus normally settles head downward into the pelvic cavity. On the completion of gestation, labour starts, it causes labour pains.
Labour period is divided into three stages :
1. Stage of Dilation : The time from the onset of labour pain to the complete dilation of the cervix is called the first stage of labour. It lasts for 6-12 hours. During this, regular contractions of the uterus, usually rupturing of the amniatic sac and complete dilation of the cervix take place. The first result of labour pains is the opening of the cervix. The amniotic fluid starts flowing out through vagina.
2. Stags of Expulsion: It is the period from complete cervical dilation to delivery of the baby. It lasts for about 20 minutes to one hour. The uterine contractions become more powerful and are accompained by contractions of the abdominal wall. With these contractions the baby is gradually pushed outward through the dilated cervix, and vagina. The umbilical cord is ligated at two places close to the baby and cut between the ligatures. This free baby totally from the mother.
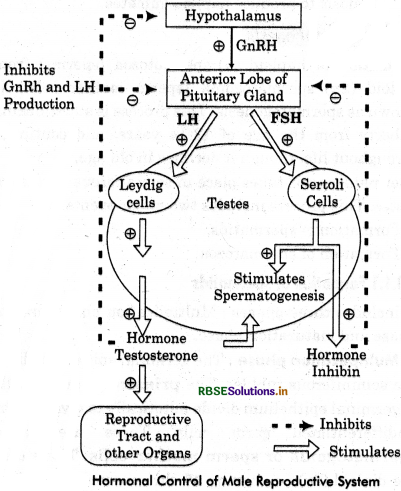
Carvix and vagina are dilated and the ligaments of the pelvic girdle are relaxed by the hormone relaxin from the corpus luteum for easy birth of the young one.
3. Placental Stage or After Birth Stage : The time after delivery until the placenta is expelled by powerful uterine constructions is the placental stage. It lasts for 10-45 minutes after the baby birth. After a few minutes the birth of baby, the uterus begins to shrink. This frees the implantation site. Now, the placenta, unbilical cord and foetal membranes are expelled by another series of uterine contractions. Within 28 - 36 days the uterus returns fully to its non-pregnant state by reduction in size and restoration of endometrium.
Question 16.
What is twins? Give the types of twins.
Answer:
Normally, a women gives birth to one baby at a time. But sometimes two or more babies also born from a mother. Such babies are called twins or multiple birth.
There are three types of twins :
1. Fraternal Twins: At a time, two eggs, one from each ovary, may be released simultaneously. And if both are fertilized, each by a separate sperm, each formed zygote develops into a yaung one. Such babies are genetically different because each receives gene from a separate egg and a separate sperm. They may be of the same or different sexes. They are known as non-identical or fraternal twins. They are more appropriately called dizygotic twins.
2. Identical Twins: If a single early zygote divides before their fate is fixed, each can develop into a complete young one. Both of the foetus formed in this manner have the same genetic make up as they have the genes of the same ovum and same sperm. They are always of the same sex, have identical characters and are almost indistinguishable. They are now more appropriately known monozygotic twins.
3. Siamese Twins: Partial separation of the two blastomers formed by zygotis first cleavage produces Siamese or conjoined twins, i.e., twins joined together at certain places.

- RBSE Class 12 Biology Notes Chapter 16 पर्यावरण के मुद्दे
- RBSE Class 12 Biology Notes Chapter 15 जैव-विविधता एवं संरक्षण
- RBSE Class 12 Biology Notes Chapter 14 पारितंत्र
- RBSE Class 12 Biology Notes Chapter 13 जीव और समष्टियाँ
- RBSE Class 12 Biology Notes Chapter 12 जैव प्रौद्योगिकी एवं उसके उपयोग
- RBSE Class 12 Biology Notes Chapter 11 जैव प्रौद्योगिकी-सिद्धांत व प्रक्रम
- RBSE Class 12 Biology Notes Chapter 10 मानव कल्याण में सूक्ष्मजीव
- RBSE Class 12 Biology Notes Chapter 9 खाद्य उत्पादन में वृद्धि की कार्यनीति
- RBSE Class 12 Biology Notes Chapter 8 मानव स्वास्थ्य तथा रोग
- RBSE Class 12 Biology Notes Chapter 7 विकास
- RBSE Class 12 Biology Notes Chapter 6 वंशागति के आणविक आधार