RBSE Class 11 Biology Important Questions Chapter 19 Excretory Products and their Elimination
Rajasthan Board RBSE Class 11 Biology Important Questions Chapter 19 Excretory Products and their Elimination Important Questions and Answers.
RBSE Class 11 Biology Chapter 19 Important Questions Excretory Products and their Elimination
Multiple Choice Questions
Question 1.
A bird excrete nitrogenous waste material in the form of:
(a) uric acid
(b) ammonia
(c) urea
(d) amino acid
Answer:
(a) uric acid

Question 2.
Which of the following are metabolic wastes of protein metabolism?
(a) Urea, oxygen and N2
(b) Urea, NH3 and CO2
(c) Ammonia, urea and creatinine
(d) Nitrogen, urea and CO2
Answer:
(c) Ammonia, urea and creatinine
Question 3.
ADH acts on the:
(a) collecting tubules of kidney
(b) loop of Henle
(c) collecting ducts of testes
(d) none of the above
Answer:
(a) collecting tubules of kidney
Question 4.
Excretory product of spider is:
(a) uric acid
(b) ammonia
(c) guanine
(d) none of these
Answer:
(c) guanine
Question 5.
Bidders canal is found in:
(a) Testes of frog
(b) Kidneys of Frog
(c) Kidneys of rabbit
(d) Both (a) and (c)
Answer:
(b) Kidneys of Frog
Question 6.
Deamination occurs in:
(a) Kidney
(b) Liver
(c) Nephron
(d) Both (a) and (b)
Answer:
(b) Liver
Question 7.
Loop of Henle is found in:
(a) Lung
(b) Liver
(c) Neuron
(d) Nephron
Answer:
(d) Nephron
Question 8.
Green glands, present in some arthropods, help in:
(a) Respiration
(b) Excretion
(c) Digestion
(d) Reproduction
Answer:
(b) Excretion
Question 9.
Which of the following is concerned with the formation of urea in rabbit:
(a) Blood
(b) Kidney
(c) Spleen
(d) Liver
Answer:
(d) Liver
Question 10.
The pH of human urine is approximately:
(a) 6.5
(b) 7
(c) 6
(d) 7.5
Answer:
(c) 6
Question 11.
Which of the following pairs is wrong?
(a) Uricotelic: Birds
(b) Ureotelic: Insects
(c) Ammonotelic: Tadpole
(d) Uriotelic: Elephant
Answer:
(b) Ureotelic: Insects
Question 12.
A person is undergoing prolonged fasting. His urine will be found to contain abnormal quantities of:
(a) Fats
(b) Amino acids
(c) Glucose
(d) Ketones
Answer:
(d) Ketones

Question 13.
Which are the components of ornithine cycle:
(a) Ornithine, citrulline and alanine
(b) Ornithine, citrulline and arginine
(c) Ornithine, alanine and fumaric acid
(d) Orinithine, citrulline and fumaric acid
Answer:
(b) Ornithine, citrulline and arginine
Question 14.
Malpighian tubules are:
(a) excretory organs of insect
(b) excretory organs of frog
(c) respiratory organs of insects
(d) endocrine glands of insects
Answer:
(a) excretory organs of insect
Question 15.
Podocytes are the cells present in:
(a) cortex of nephron
(b) inner wall of Bowman’s capsule
(c) outer wall of Bowman’s capsule
(d) wall of glomerular capillaries
Answer:
(b) inner wall of Bowman’s capsule
Question 16.
The net pressure gradient that causes the fluid to filter out of the glomeruli into the capsule is:
(a) 50 mm Hg
(b) 75 mm Hg
(c) 20 mm Hg
(d) 30 mm Hg
Answer:
(c) 20 mm Hg
Question 17.
Earthworms are:
(a) Ammonotelic when plenty of water is available
(b) Ureotelic when plenty of water is available
(c) Uricotelic when plenty of water is available
(d) Uricotelic under conditions of water scarcity
Answer:
(a) Ammonotelic when plenty of water is available
Question 18.
Excretory organs in flat worms are:
(a) flame cells
(b) nephridia
(c) malpighian tubules
(d) ranette glands
Answer:
(a) flame cells
Question 19.
Excretion in cockroach occurs through:
(a) Nephridium
(b) Parotid gland
(c) Coxal gland
(d) Malpighian tubules
Answer:
(d) Malpighian tubules
Question 20.
Uric acid is formed from:
(a) Protein
(b) Pyrimidines
(c) Purines
(d) Glucose
Answer:
(c) Purines
Question 21.
Renin is released by:
(a) Cortical nephron
(b) Collecting duct.
(c) Juxtaglomerular apparatus
(d) Pelvis
Answer:
(c) Juxtaglomerular apparatus
Question 22.
Absorption of water in DCT is controlled by:
(a) ACTH
(b) ADH
(c) LH
(d) Oxytocin
Answer:
(b) ADH
Question 23.
Which one produces erythropoietin:
(a) Kidney
(b) Pancreas
(c) Pineal body
(d) Thyroid
Answer:
(a) Kidney
Question 24.
During summer, which hormone concentration is maintained at high level:
(a) Insulin
(b) Vasopressin
(c) Oxytocin
(d) Corticoid
Answer:
(b) Vasopressin
Question 25.
Maximum amount of electrolytes and 70 - 80% water from glomerular filtrate is absorbed in:
(a) PCT
(b) Descending limb of loop of Henle
(c) Ascending limb of loop of Henle
(d) DCT
Answer:
(a) PCT
Question 26.
How much urea is reabsorbed from tubular filtrate:
(a) 20%
(b) 50%
(c) 100%
(d) It is not absorbed at all
Answer:
(b) 50%
Question 27.
Bowman’s capsule is a part of:
(a) Ureter
(b) Renal artery
(c) Renal portal vein
(d) Uriniferous tubule
Answer:
(d) Uriniferous tubule
Question 28.
Detrusor muscles are present in:
(a) Liver
(b) Kidney
(c) Urinary bladder
(d) Ureters
Answer:
(c) Urinary bladder
Question 29.
Excretory organs of Ascaris is:
(a) Solenocytes
(b) Green glands
(c) Hatschsk nephridium
(d) Renette cells
Answer:
(d) Renette cells
Question 30.
Ornithine cycle takes place in:
(a) Kidney
(b) Liver
(c) Heart
(d) Muscles
Answer:
(b) Liver
Question 31.
Which of the following is a nitrogenous waste?
(a) Creatine
(b) Guanine
(c) Uric acid
(d) All of these
Answer:
(d) All of these

Question 32.
Erythropoietin helps in:
(a) Urea synthesis
(b) Blood synthesis
(c) Blood disintegration
(d) Disintegration of RBCs in liver
Answer:
(b) Blood synthesis
Question 33.
Which one of the following is not a part of a renal pyramid:
(a) Loop of Henle
(b) Collecting ducts
(c) A convoluted tubules
(d) Peritubular capillaries
Answer:
(c) A convoluted tubules
Question 34.
Fresh water bony fishes maintain water balance by:
(a) excreting a hypotonic water
(b) drinking small amount of water
(c) excreting salts across their gills
(d) excreting wastes in form of uric acid
Answer:
(a) excreting a hypotonic water
Question 35.
The principal nitrogenous excretory compound in humans is synthesised in:
(a) Kidneys as well as eliminated by kidneys
(b) Liver, but eliminated mostly through kidneys
(c) Kidneys but eliminated mostly through liver
(d) Liver and also eliminated by the same through bile
Answer:
(b) Liver, but eliminated mostly through kidneys
Question 36.
The amino acid that acts as a carrier of ammonia from skeletal muscles to liver:
(a) Alanine
(b) Methionine
(c) Arginine
(d) Glutamine
Answer:
(d) Glutamine
Question 37.
Urea synthesis takes place primarily in liver because:
(a) Enzyme arginase is present in liver only
(b) NH3 and CO2 are present in liver only
(c) Hormone ADH is found in liver only
(d) Kidney is smaller than liver
Answer:
(a) Enzyme arginase is present in liver only
Question 38.
Filtration of the blood takes place in:
(a) PCT
(b) DCT
(c) Collecting ducts
(d) Malpighian body
Answer:
(d) Malpighian body
Question 39.
Which one of the following statement in regard to the excretion by the human kidney is correct:
(a) Descending limb of loop of Henle is impermeable to water
(b) DCT is incapable of reabsorbing HCO3
(c) Nearly 99% of the glomerular filtrate is reabsorbed by the renal tubules
(d) Ascending limb of loop of Henle is impermeable to electrolytes
Answer:
(c) Nearly 99% of the glomerular filtrate is reabsorbed by the renal tubules
Question 40.
The part of a nephron which opens into the collecting duct is/are:
(a) DCT
(b) Glomerulus
(c) Henle's loop
(d) DCT & PCT
Answer:
(a) DCT
Very Short Answer Type Questions
Question 1.
What is the pH of urine?
Answer:
6
Question 2.
What are podocytes?
Answer:
Epithelial cells of Bowman’s capsule are called podocytes.
Question 3.
Name the excretory organ of cockroach.
Answer:
Malpighian tubules.

Question 4.
Name the hormone which controls the concentration of sodium in the body.
Answer:
Aldosterone.
Question 5.
Name any two constituents of human sweat.
Answer:
Sodium chloride, lactic acid.
Question 6.
Define the Glomerular Filtration Rate (GFR).
Answer:
The amount of filtrate formed by kidney per minute.
Question 7.
Name any two types of nephrons found in human kidney?
Answer:
Juxta medullary nephrons and cortical nephrons.
Question 8.
What is micturition?
Answer:
The act of voiding out of urine from urinary bladder.
Question 9.
Write the function of renin produced by kidney.
Answer:
Renin convert the angiotensinogen into angiotensin.
Question 10.
What is angiotensinogen?
Answer:
It is a plasma protein.
Question 11.
Name the excretory organs of Ascaris?
Answer:
Renette cells.
Question 12.
Name the excretory products of reptiles.
Answer:
Uric acid.
Question 13.
What is glomerulus?
Answer:
It is a tuft of capillaries present in Bowman’s capsule.
Question 14.
What do you mean by ureotelic?
Answer:
The animals which excrete urea are called ureotelic.
Question 15.
What do you mean by aminotelic animals?
Answer:
The animals excreting amino acids.
Question 16.
Give any two examples of aminotelic animals.
Answer:
Pila and starfish.
Question 17.
Name the excretory organ of pila.
Answer:
Organs of Bojanus.
Question 18.
Where does ornithine cycle occur?
Answer:
In liver.
Question 19.
Who coined the term homeostasis?
Answer:
Walter Cannon.
Question 20.
Where do podocytes occur?
Answer:
In the lining of inner wall of Bowman’s capsule.
Question 21.
What is polyuria?
Answer:
Production of unusually excess amount of urine.
Question 22.
What is Dysuria?
Answer:
Painful urination.
Question 23.
What do you mean by oligouria?
Answer:
A condition of production of less urine.
Question 24.
Name the condition of excessive urination at night.
Answer:
Nocturia.
Question 25.
What is gout?
Answer:
It is a uric acid disorder in which uric acid gets deposited in joints to make them painful.
Question 26.
What are solenocytes?
Answer:
Flame cells of cephalochordates.
Question 27.
Name the excretory organs of earthworm.
Answer:
Nephridia.
Question 28.
What is ANF?
Answer:
Atrial natriuretic factor.
Question 29.
Where does the formation of angiotensinogen takes place?
Answer:
In liver.

Question 30.
What do you mean by Renal calculi?
Answer:
Stone or insoluble mass of crystallised salts formed with in the kidney?
Question 31.
What are columns of Bertini?
Answer:
The cortex extends in. between the medullary pyramids as real columns called columns of Bertini.
Question 32.
What is glomerulonephritis?
Answer:
Inflammation of glomeruli of kidney.
Short Answer Type Questions
Question 1.
What do you mean by peritubular capillary network.
Answer:
Peritubular capillary network is formed when a minute vessel of peritubular capillaries runs parallel to the loop of Henle forming a ‘U’ shaped vasa recta.
Question 2.
What is difference between descending and ascending limbs?
Answer:
|
Descending Limb |
Ascending Limb |
|
1. It is very thin. |
1. It is thick. |
|
2. Direction of fluid flow is downward. |
2. Direction of fluid flow is upward. |
|
3. Permeable to water. |
3. Impermeable to water. |
Question 3.
Write the differences between cortical and juxtamedullary nephron.
Answer:
|
Cortical Nephron |
Juxtamedullary Nephron |
|
1. These are large in number and forms about 80% of the total nephrons. |
1. These are small in number and form about 20% of the total nephrons. |
|
2. Loop of Henle is too short. |
2. The loop of Henle is very long. |
|
3. They extend only very little into the medulla i.e., lie in the renal cortex. |
3. There Henle’s loop runs deep into the medulla. |
Question 4.
What do you mean by Juxtaglomerular apparatus?
Answer:
Juxtaglomerular apparatus (JGA) is a special sensitive region formed by cellular modifications in the distal convoluted tubule and the afferent arteriole at the location of their contact.
Question 5.
What is the role of counter-current mechanism in the excretion?
Answer:
The counter current mechanism helps in the maintenance of a concentration gradient in the medullary interstitium. Presence of such gradient helps in an easy passage of water from the collecting tubule resulting in the formation of concentrated urine (filtrate) i.e., nearly four times concentrated than the initial filtrate formed.

Question 6.
Write the difference between the tubular reabsorption and tubular secretion.
Answer:
|
Tubular Reabsorption |
Tubular Secretion |
|
1. It involves the absorption of water and useful solutes |
1. It refers to the passage of waste material from blood into the filtrate of nephrons. |
|
2. It occurs by back diffusion and active transport. |
2. It takes place only by active transport. |
|
3. It occurs mostly in PCT. |
3. It occurs mostly in DCT. |
|
4. It does not occur in animals that lack glomerulus e.g., marine fishes and desert animals. |
4. It is the only mode of excretion in animals that lack glomerulus. |
Question 7.
Why the excretory wastes occur in human being are mostly nitrogenous compounds?
Answer:
Because human body can store carbohydrates and fats for future use but can not store proteins or amino acids. So harmful amino acids must be removed from the body. Therefore, the amino acids which are not in use are deaminated that regulates the formation of nitrogenous wastes.
Question 8.
What are the cmponents of juxta glomerular apparatus? How does it work?
Answer:
Juxta glomerular apparatus contain includes:
- Granular juxtaglomerular cells in the afferent arteriole.
- Macula densa cells of DCT.
- A granular lacis cells situated in between the above two.
A fall in GFR can activate the Juxtaglomerular cells to release renin, which can stimulate the glomerular blood flow and thereby, the GFR back to normal.
Question 9.
What is the difference between renin and rennin?
Answer:
|
Renin |
Rennin |
|
1. It is secreted by juxtag - lomerular cells of JGA. |
1. It is secreted by peptic cells of gastric gland. |
|
2. It is secreted as renin. |
2. It is secreted in the form of |
|
3. It is considered as hormone because it is secreted from endocrine part of JGA. |
3. It is a protein digestive enzyme. |
Question 10.
What is the difference between sweat and sebum?
Answer:
|
Sweat |
Sebum |
|
1. It is secreted from the sweat gland or sudoriferous glands of skin. |
1. It is secreted from sebaceous or oil glands of the skin. |
|
2. Its secretion is stimulated by rise in body temperature. |
2. Its secretion takes place continuously. |
|
3. Secretion is watery. |
3. Secretion of oily. |
|
4. It helps in lower the body temperature by cooling the surface of skin. |
4. It forms a protective covering and prevent the skin from drying. |
Question 11.
Why is it not advised to drink lot of water after heavy sweating?
Answer:
During heavy sweating, body loses lot of salts. If lot of water is taken after heavy sweating, it will dilute the tissue fluid causing electrolyte imbalance in the body.
Long Answer Type Questions
Question 1.
Discuss the different types of nitrogenous waste products. How is the urea formed in the mitochondria of liver cells?
Answer:
Excretory substances of animals can be classified into two categories:
Organic Waste Products: It is mainly carbondioxide. It is hamrful to cells due to its acidic nature. It is produced during cellular respiration and exhaled out by with the help of respiratory organs.
Nitrogenous Waste Products: These are nitrogen containing waste products. These are formed either by decomposition of proteins or nucleic acids.
Excretory Waste formed by Protein Metabolism:
1. Ammonia: Ammonia is produced due to deamination of aminoacids during protein metabolism. Since it is toxic so it must be eliminated immediately from the body of animal. Being highly soluble in water, it is excreted out from the body of animals. It is excretory product of protozoans, porifera, cnidarians, annelids and molluscs etc. These animals are called ammonotelic and the phenomena is called ammonotelism.
2. Urea: Urea is produced by combination of ammonia and carbon dixoide in liver during ornithine cycle. It occurs abundantly out of other excretory products. It is less toxic than ammonia. It requires less water for its removal. It is the excretory product of elasmobranchs fishes, amphibians and mammals. These animals are called ureotelic and the phenomenon is called ureotelism.
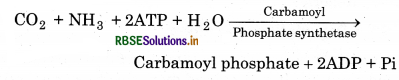
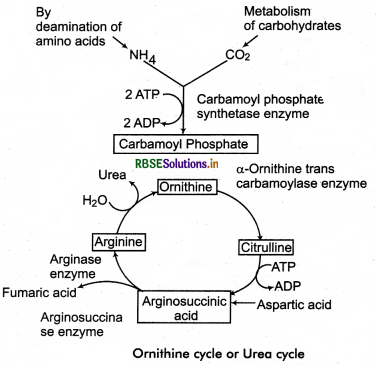
Ornithine Cycle: It occurs in the mitochondria of liver cells (hepatocytes).
It occurs in following steps
1. Ammonia (formed from deamination of amino acids) reacts with carbon dioxide and phosphate (of ATP) to form carbamoyl phosphate.
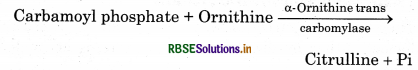
2. Now carbamoyl phosphate reacts with ornithine to form citrulline.
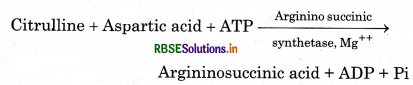
3. Citrulline and aspartic acid reacts with each other in argininosuccinic acid.
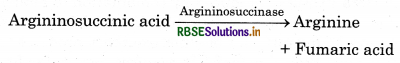
4. Argininosuccinic acid dissociates into arginine and fumaric acid in presence of argininosuccinase enzyme.
5. Arginine further dissociates into urea and ornithine in presence of arginase enzyme.

1 molecule of CO2, 2 molecules of NH3 and 3 ATP are used to form 1 molecule of urea.
3. Uric Acid: In some animals, like insects, some molluscs, birds and most of reptiles, ammonia produced by protein catabolism in liver is converted to uric acid. It is insoluble in water. It is excreted in the form of solid crystals. Human excretory wastes contain 0.5% uric acid. The animals who excrete uric acid as excretory product are called uricotelic and this phenomena is called uricotelism.
Excretory wastes formed by Metabolism of Nucleic acids: Nitrogenous bases like purines and pyrimidines are produced during catabolism of nucleic acids. In human being, purines are excreted in the form of uric acid and pyrimidines are excreted in the form of alanine. Other animals excrete these in the form of allantoin and allantoic acid that are also nitrogenous wastes products.
Other Excretory Wastes:
- Creatine and Creatinin: In the body, creatin remains as a high energy compound creatin phosphate. It is excreted out in the form creatin or creatinine.
- Hippurlc acid and Ornithuric acid: It is formed by the joining of benzoic acid (which is present in mammals’s food) with glycine. In birds, benzoic acid joins with ornithine to form ornithuric acid and excreted in the said form.
- Trimethylamine oxide: It is the excretory product of marine fishes.
- Besides the above, xanthene, hypoxanthene, guanine, thymine are the excretory products of different animals.
Question 2.
Write a detail account of the excretory organs of invertebrates. How do they help in excretion?
Answer:
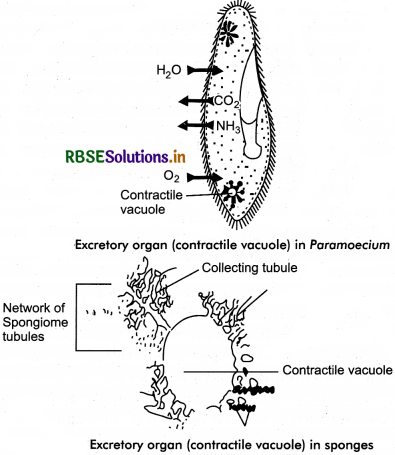
1. In Protozoans: In protozoans like Amoeba and Paramoecium, carbon dioxide and ammonia are mostly excreted out by diffusion through general body surface. It is considered that the contractile vacuoles also play some role in the removal of excretory products.
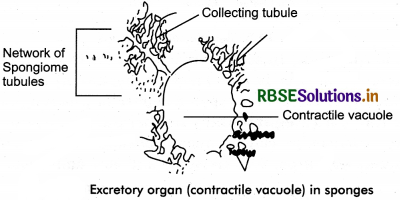
2. In sponges: In sponges, the nitrogenous metabolic waste (ammonia) leaves the body in the outgoing water current by diffusion. Most of the sponges are marine and have no problem of surplus water in their cells. A few sponges lie in hypotonic fresh water and have contractile vacuoles in most of their cells.
3. Coelenterates: Coelenterates like Hydra lacks special excretory organs. The nitrogenous waste products like ammonia are removed through the general surface of the body by diffusion. Some nitrogenous waste products are also thrown along with undigestible matter through the mouth.
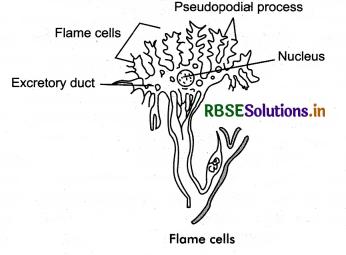
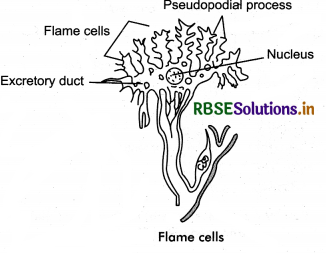
4. In platyhelminthes: Flatworms like planarians, fluke and tapeworms have flame cells (solenocytes) with bundles of vibratile cilia for excretion. The flame cells receive the solute and water from the surrounding tissue fluid by ultrafiltration and discharge the filtrate into the nephridial ducts. The final urine so formed is eliminated to the exterior by way of excretory pores.
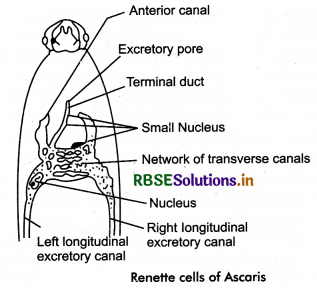
5. In Nematoda: The round worm such as Ascaris have “H” shaped excretory system. It is made up of a single Renette cell in entire length of body. It consists of two
longitudinal excretory canal connected anteriorly by a network of transverse canal. A short terminal duct opens out side through excretory pore. Ascaris excretes both
ammonia and urea.
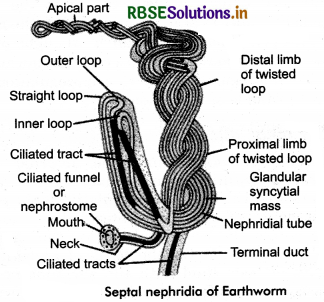
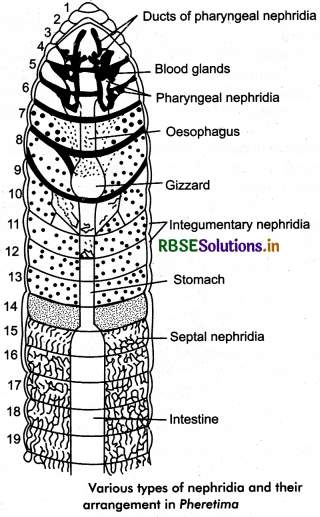
6. In Annelids: In some annelids like Earthworm, the excretory system is also known a nephridial system, which consists of three types of nephridia - pharyngeal, septal and Integumentary nephridia. All nephridia are commonly called micronephridia. Earthworm excrete 40% urea, 20% ammonia and 40% amino acids.
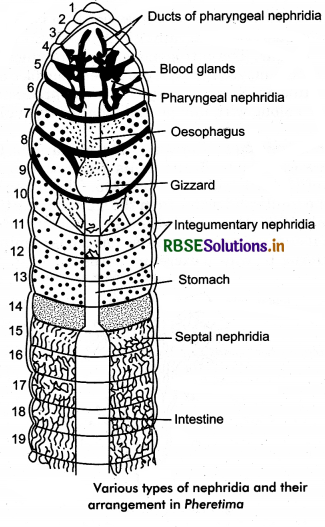
Earthworm is mainly ureotelic. Chioragogen cells found in coelomic fluid also excretory in nature. Blood gland in earth worm found m 4th, 5th, 6th segment, serves for excretion, manufacture of blood corpuscles and haemoglobin.
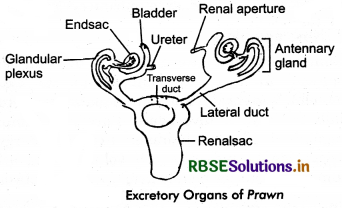
7. In arthropods: The excretory system of the adult prawn (crustacean) consists of a pair of antennary or green glands, a pair of lateral ducts and a single renal sac. Insects, centipedes, milipedes and arachnoids like scorpion and spider possess malpighian tubules as their principal excretory organs. In the malpighian tubules, bicarbonates of potassium and sodium are reabsorbed by the cells of Malpighian tubules and then transferred to the blood (haemolymph). Uric acid is carried to the alimentary canal of the insect and is finally passed out through anus. Spiders and scorpions possess Malpighian tubules and coxal glands both for excretion.
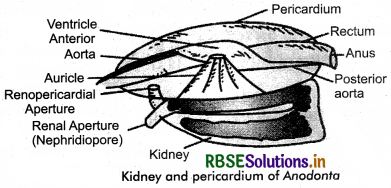
8. In Molluscs: Molluscs have 1 or 2 pairs of kidneys for excretion. The kidneys opens into the pericardium (coelom) at one end by renopericardial aperture (nephrostome) and into the mentie cavity at the other end by nephridiopore. The auricular wall forms pericardial fluid (primary urine) by ultrafiltration across it. In the kidney the primary urine is modified to final urine by selective reabsorption and excretion. The final urine passes into mentie cavity via nephridiopore. The waste matter is ammonia is aquatic forms and uric acid in land forms. The kidneys perheps carry on osmoregulation also in fresh water forms.
9. In Echinoderms: In echinoderms like starfish, specialised excretory organs are absent. The excretory products chiefly ammonia, urea and creatinine are eliminated by diffusion through dermal branchiae (primitive gills) and tube feet. Amoeboid coelomocytes are also excretory in function.

Question 3.
Draw the diagram of the following:
(a) Flame cell of tapeworm.
(b) Renette cell of Ascaris.
(c) A septal nephridium of earthworm.
Answer:
(a)
(b)
(c)
Question 4.
Write a detailed account of human excretory system.
Answer:
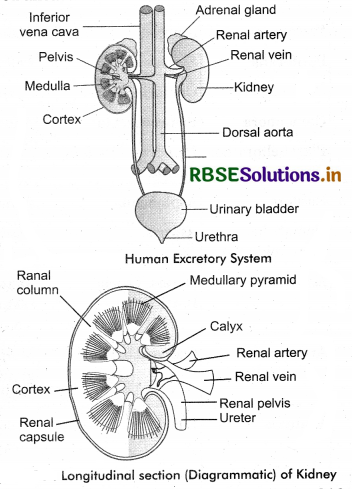
Human excretory system consists of a pair of kidneys, a pair of ureters, urinary bladder and urethra.
Kidneys: The kidneys are bean - shaped, reddish brown paired organs, concave on one long side and convex on the opposite.
Location: They are normally located on upper side (anterior part) in abdominal cavity and against its back wall (dorso laterally) lying on either side of the vertebral column between the levels of the 12th thoracic and third lumber vertebrae and outside the peritoneum, the membrane that lines the abdomen.
Size: Each kidney of an adult human measures about 10 - 12 cm in length, 5 - 7 cm in width, 2 - 3 cm in thickness with an average weight of 120 - 170 g.
External Structure of Kidney: The outer surface of each kidney is convex and inner surface is concave where it has a depression called Hilum, through which the renal arteries and renal veins enter and leave the kidney along with the ureter and the nerve supply of kidney. There are three protective covering occurs from outside to inside of each kidney:
- Renal Fascia: It is outermost and fibrous covering of each kidney. It help to anchored the kidney with abdominal wall.
- Adipose layer: It is middle covering, composed of adipose (fat) tissues. It acts as a shock absorber.
- Renal capsule: It is the innermost covering. It is actual covering made up of white fibrous connective tissue with a few yellow elastic fibres and few muscles. It also protects the kidney from the external shocks and infections.
Infernal Structure of Kidney:
There are three major regions in the internal structure of kidney:
- Renal cortex
- Renal Medulla
- Renal Pelvis
The renal cortex is a space between the medulla and the outer capsule. The renal medulla contains the majority of the length of nephron (the main functional component of kidney that filters fluid from blood). The renal pelvis connects the kidney with the circulatory and nervous system from the rest of the body.
Renal Cortex: It is a layer of tissue covered by renal fascia and the renal capsule. It appears agranular due to presence of nephron (functional unit of kidney) that are located deeper within the kidney, within the renal pyramids of the medulla. The cortex provides a space for arterioles and venules from the renal artery and vein, as well as the glomerular capillaries, to perfuse the nephrons of the kidney.
Erythropoitin, a hormone necessary for the synthesis of new red blood cells, is also produced in the renal cortex.
Renal Medulla: This part consists of multiple pyramidal tissue masses, called the renal pyramids which are triangular structures containing a dense network of nephrons. Broad base of conical renal pyramid remains towards the cortex while pointed apex towards the medulla. The pointed end of renal pyramid is called renal papilla (PI = papillae). 1 - 3 renal papillae projects into a cavity called minor cay lx. Minor calyces (singular = calyx) join to form 2 - 3 major calyces. The major calyces in turn, opens into a wide, funnel - like structure called pelvis. The renal pelvis leads into the ureter.
The cortex projects into the medulla in the regions between pyramid and calyces. These cortical projections are called renal columns of Bertini. The cortex region that lies close to medulla is called juxtamedullary area. As we stated formerly in this heading that a renal pyramid contains a dense network of nephron which is structural and functional unit of kidney. The structure of nephron will be described ahead.
Functions of Kidney: With the help of nephrons, kidney performs following homeostatic functions:
- Maintain volume of extracellular fluid.
- Maintain ionic balance in extracellular fluid.
- Maintain pH and osmotic concentration of extracellular fluid.
- Excrete toxic metabolic by products such as urea, ammonia and uric acid.
2. Ureters: These tube arises from the hilum of each kidney, run downwardly to join with urinary bladder. They are made of smooth muscle fibres. They propel urine from the kidneys to the urinary bladder. In adult human, the ureters are 25 - 30 cm long and around 3 - 4 mm in diameter. Each ureter is lined by urothelial cells, a type of transitional epithelium, and has an additional smooth muscle layer in the more distal one - third to assist with peristalsis. Urine produced by the kidneys travels along the ureters to the bladder with the help of peristalsis.
3. Urinary Bladder: The urinary bladder is a temporary storage reservoir for urine. It is located in the pelvic cavity, posterior to the pubic symphysis and below the parietal peritoneum. The size and shape of the urinary bladder varies with the amount of urine it contains and with the pressure it receives from surrounding organs. The wall of urinary bladder contains of 3 coats:
(A) The inner lining of urinary bladder is a mucous membrane of transitional epithelium that is continuous with that in the uterus. When the bladder is empty, the mucous has numerous folds called rugae. The rugae and transitional epithelium allow the bladder to expand as it fills.
(B) The second layer in the walls is submucosa which supports the mucous membrane. It is composed of connective tissue with elastic fibres.
(C) The next layer is the muscularis, which is composed of smooth muscles. The smooth muscle fibres are interwoven in all directions and collectively these are called detrusor muscle, contraction of these muscles expels urine from the bladder.
On the superior surface, the outer layer of bladder wall is parietal peritoneum. In all other regions, the outer layer is fibrous connective tissue.
There is a triangular area, called trigone formed by three openings in the floor of the urinary bladder. Two
of the openings are from the ureters and form the base of trigone. Small flaps of mucosa cover these openings and acts as valves that allow urine to enter the bladder but prevent it from backing up from the bladder into the ureters. The third opening, at the apex of trigone, is the opening into the urethra. A band of the detrusor muscle encircles this opening to form the internal urethral sphincter.
4. Urethra: It is a thin walled tube that coveys urine from the floor of the urinary bladder to the outside. The opening to the outside is the external urethral orifice. The mucosal lining of urethra is transitional epithelium. The wall also contains smooth muscle fibres and is supported by connective tissues. The internal urethral sphincter surrounds the beginning of the urethra, where it leaves the urinary bladder. This sphincter is smooth (involuntary) muscle. Another sphincter, the external urethral sphincter, is skeletal (voluntary) muscle and encircles the urethra where it goes through the pelvic floor. These two sphincters controls the flow of urine through the urethra. In females, the urethra is short, only 3 - 4 cm long. The external urethral orifice opens to the outside just anterior to the opening for the vagina.
In males, the urethra is much larger, about 20 cm in length, and transports both urine and semen. It can be divided into 3 parts:
- Prostative urethra : It is the first part, next to the urinary bladder, passes through the prostate gland.
- Membranous urethra: The second part that penetrates the pelvic floor and enters the penis. It receives the ejaculatory ducts and opening of Cowper’s gland.
- Penile urethra: It is the longest part that extends the entire length of the penis, and the external urethral orifice opens to the outside at the top of the penis.
Supply of Blood and Nerves to the Kidneys
Each kidney is supplied with blood via renal artery and drained the blood by renal vein.
Renal Artery: The renal artery enters the kidney via the renal hilum. Inside the kidney it divide and redivide to gives of afferent arterioles. The afferent arterioles form a capillary network, the glomerulus where filtration takes place. The capillaries come together to form the efferent arterioles.
In the outer two - thirds of the renal cortex, the efferent arterioles forms a peritubular capillary network (P.T.C.N.) in the cortex around the proximal and distal convoluted tubules of the nephron. From the peritubular capillaries arises the capillaries of vasa recta which extend parallel to the loops of Henle and the collecting ducts in the medulla.
Renal Vein: All the capillary networks return blood containing useful materials to the renal venules which join to form a renal vein that opens into the inferior vena cava.
Question 5.
Draw a neat & clean figure showing the structure of nephron. Discuss the different parts of nephron giving the function of each.
Answer:
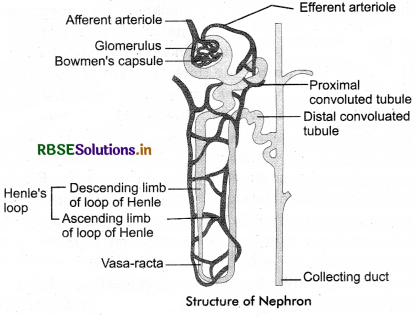
Each kidney is composed of numerous (nearly one million) complex tubular structure called nephrons. Each nephron is about 3 cm long and thus they form a large surface area (about 80 km) for the exchange of materials in the kidney.
Types: Based on the location in the kidney, nephrons are of following two types:
1. Cortical Nephrons: In majority of nephrons, the loop of Henle is too short and extends only very little into the medulla i.e., lie in the renal cortex. Such type of nephrons are called cortical nephrons.
Glomerutus: The glomerulus is a capillary network that arises from an afferent arteriole and empties into an efferent arteriole. The diameter of efferent arteriole is smaller than that of the afferent arteriole which helps to maintain a fairly high blood pressure in the glomerulus. The wall of both afferent and efferent arteriole possess specialised cells called juxtaglomerular cells. These cells produce renin and erythropoietin.
Bowman’s Capsule or Glomerutar Capsule: It is double walled, cup - like structure and it encloses the glomerulus. The wall of glomerulus and the Bowman’s capsule consists of a single layer of flattened epithelial cells.
Bowman’s capsule consists of three layers:
(i) Outer Parietal Layer: It consists of flat, squamous epithelial cells with minute pore of 12 nm diameter called fenestrations.
(ii) Middle Basement Membrane: It is selectively permeable membrane lies between parietal and visceral layer.
(iii) Inner Visceral Layer: It consists of large nucleated cell called podocytes. Podocytes bear finger like projections called pedicels or feet. The pedicels rest over the basement membrane. They encloses slit pores or filtration slits. The diameter of these slits is about 25 nm. Pedicels also poosses contractile filaments which helps in passage of filterate through the filtration slits.
2. Renal tubules: The renal tubule continues from Bowman’s capsule and consists of the following parts:
- Proximal convoluted tubules (P.C.T.).
- Loop of Henle.
- Distal convoluted tubules (D.C.T.)
- Connecting tubules.
(i) Proximal Convoluted Tubules (P.C.T.): It is proximal part of renal tubules next to Bowman’s capsule. It is surrounded by peritubular blood capillaries. P.C.T. is lined by cuboidal epithelium. Cells of cuboidal epithelium usually becomes cone - shaped. They possess brush borders with long microvilli for increasing absorptive area. The cells contain abundant mitochondria and reserve food for providing energy to perform active absorption and secretion. Terminal end of PCT is Descending of limb is Henle’s loop non convoluted. It is called as parsrecta. Maximum reabsoption of water, glucose, amino acids and electrolytes takes place here.
(ii) Loop of Henle: It is ‘U’ shaped middle portion of renal tubules. It has two parallel limbs - a descending limb which is continuation of PCT into the renal medulla and ascending limb that re-enters the renal cortex and remains continue as DCT. Each limb has a thick region towards the cortex and a thin region on the other side. The thick regions are lined by columnar cells and the thin regions by flat cells.
(iii) Distal Convoluted Tubules (DCT): It is last part of nephron occurs in cortex. DCT is lined by cuboidal cells having sparse microvilli and deep mitochondria. But the part of DCT which lies close to Malpighian body has closely packed (dense) specialised cells. This is called macula densa. The cells of macula densa are sensitive to the concentration of sodium chloride in the DCT. Some workers believe them to produce renin just like juxta glomerular cells. DCT is covered by peritubular capillary network. The last part of DCT is nearly straight and called connecting or junctional tubule. Connecting tubule leads to collecting duct.
Collecting duct: Collecting duct is larger duct which receives many connecting tubules of several nephrons. Collecting ducts pass into the renal medulla and join with each other to form the ducts of Bellini. The ducts of Bellini runs through the renal pyramid and opens into calyces. All calyces open into the pelvis. From the pelvis, urine is carried to the urinary bladder through the ureters. The collecting ducts are lined by cuboidal and columnar epithelium.
Question 6.
Give an account of the physiology of excretion. Discuss the major steps which helps in the formation of urine.
Answer:
Mechanism of urine formation involves 3 processes:
- Glomerular filtration.
- Tubular reabsorption
- Tubular secretion
1. Glomerular filtration: The first step of urine formation is the filtration of blood, which is carried out by glomerulus thus it is also called glomerular filtration. On an average 1100-1200 mL of blood is filtered by the kidneys per minute which constitute roughly l/5th of the blood pumped out by each ventricle of the heart in a minute.
The glomerular capillary blood pressure causes filtration of blood through 3 layers, i.e., the endothelium of glomerular blood vessels, the epithelium of Bowman’s capsule and a basement membrane between these two layers. The epithelial cells of Bowman’s capsule called podocytes are arranged in an intricate manner so as to leave some minute spaces called filtration slits or slit pores. Blood is filtered so finely through these membranes, that almost all the constituents of the plasma except the protein pass on to the lumen of the Bowman’s capsule. Therefore, it is considered as a process of ultrafiltration. The filtered out fluid is known as ultrafiltrate as glomerular filtrate.
Mechanism of Ultrafiltration: The blood enters the glomerulus through afferent arteriole and leaves by efferent arteriole. The afferent arteriole has wider A, lumen then efferent arteriole. Hence, the blood pressure p in glomerular capillaries becomes very high so there is continuous process of filtration under pressure. Thus, water and many dissolved substances from the blood are filtered into the lumen of Bowman’s capsule through its wall. The afferent arterioles supplying blood to glomerular capsule carries useful as well as harmful substances.
The useful substances are glucose, amino acids, vitamins, hormones, electrolytes, ions etc., and the harmful substances are metabolic wastes such as urea, uric acids, creatinine, ions etc. Molecules smaller than 3 nm (such as water, glucose, amino - acids and nitrogenous wastes) in diameter pass easily to renal tubule, larger molecules pass with difficulty whereas molecules greater than 7 - 9 nm cannot pass to renal tubule. The net filtration pressure (NFP) is T responsible for filterate formation.
2. Tubular Reabsorption: A comparison of the volume of the filterate formed per day (180 liters per day) with that of the urine released (1.5 litres), suggest that nearly 99% of the filterate has to be reabsorbed by the renal tubules. This process is called reabsorption. The tubular 3 epithelial cells in different segments of nephron performs this either by active or passive mechanism. Substances like glucose, amino acids, Na+ etc., in the filtrate are reabsorbed actively whereas the nitrogenous wastes are absorbed by passive transport. Reabsorption of water also occurs passively in the initial segment of the nephron.
Reabsorption is influenced by:
- Parathormone and calcitonin hormones regulate reabsorption of calcium and phosphate.
- Antidiuretic hormone (ADH) affects the permeability of DCT and collecting tubules and regulate water absorption.
- Aldosterone (from adrenal cortex) influence reabsorption of sodium and excretion of potassium.
3. Tubular Secretion: It is the selective process involving both passive and active transport. As the blood travels through glomerulus, some harmful/unwanted substances may not be cleared from the blood by filtration because of short time. Such substances are cleared by secretion into the convoluted tubules (PCT and DCT). Substances like H+, K+, NH4, ceactinine, certain organic acids and medicines (penicillin, aspirin etc.) move either from blood of the peritubular capillaries through the tubule cells or directly from the tubule cells into filtrate. Thus, urine eventually excretes fitered and secreted substances. Tubular secretion is also important to maintain blood pH.
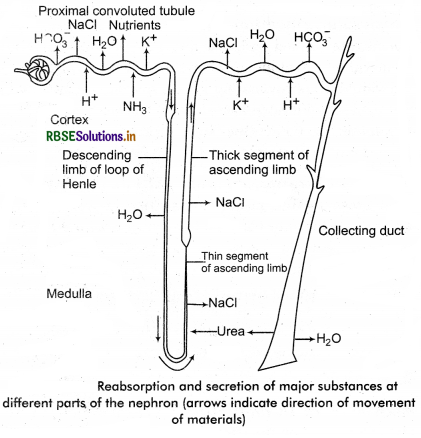
Functions of the Tubules: When the glomerular filtrate/ primary urine passes through renal tubule, water and different materials of filtrate reabsorb at various places. These are described as under.
1. Proximal Convoluted Tubule (PCT) : The epithelial cells of the PCT have numerous microvilli (simple cuboidai brush border epithelium) which increases the surface area available for reabsorption. In this part, sugars (glucose etc.), vitamins, amino acids and other organic nutrients are reabsorbed. Major amount of water is also reabsorbed by PCT. Na+ ions, Cl- ions and bicarbonate ions are reabsorbed in PCT. Henle’s loop and DCT. About 2/3rd of Na+ reabsorption occurs in PCT alone. K+ is also reabsorbed from PCT. About 53% of the urea is reabsorbed in the various parts of nephron and only 47% of the filtered urea is passed out with the urine. Some part of urea is reabsorbed in PCT while rest is reabsorbed from collecting tubules.
2. Henle's loop: Reabsorption in Henle’s loop is minimum besides it, this play an important role in maintaining the high osmolarity of medullary interstitial fluid. Two portions of Henle’s loop play different role in osmoregulation which is given below:
(a) Descending limb: The thick segment of descending limb located in both sides partly in cortex and some in medulla. The thin segment (narrow part) of descending limb lies in medulla. Thick segment is nearly impermeable. Thin segment (in medulla) loses a lot of water due to osmosis and thus, it makes the filtrate hypertonic concentration of NaCl becomes high. There is no secretion in the descending limb of loop of Henle. Urea coming through secretion from medulla enters into thin segment of loop of Henle.
3. Ascending Limb: Ascending limb consists of a thin part (towards medulla) and a thick part (towards cortex). Thick segment is impermeable to water but permeable to K+, CD and Na+ and partially permeable to urea. Thus, in the thick ascending limb of the loop of Henle, Na+, K+, Mg++ and Cl- are reabsorbed. Therefore, as the concentrated filtrate pass upward, it gets diluted due to the passage of electrolytes to the medullary fluid.
4. Distal Convoluted Tubules (DCT): In this part, under the effect of ADH (vasopressin) water is reabsorbed. Na+ is also actively reabsorbed in this part by the action of aldosterone. Besides this K+ and H+ ions are mainly secreted along with small quantities of uric acid, creatinine, some ammonia and extra salts.
Collecting Ducts: This duct extend from the cortex of the kidney to the inner parts of the medulla and is highly permeabe to water. Like the DCT, water and Na+ are reabsorbed under the effects of ADH or vasopressin and aldosterone respectively. It also allows to pass a small amount of urea into the medullary interstitium to maintain the osmolarity. It also plays an important role in the maintenance of pH and ionic balance of blood by selective secretion of H+ and K+ ions. Therefore, the filtrate is now called urine. Thus, urine is isotonic to medullary fluid and hypertonic to blood. Concentrations of important ions and other substances in the blood are controlled by regulating water levels.

Question 7.
How does the function of kidney regulate? Discuss the endocrine mechanism which regulate the kidney’s functions.
Answer:
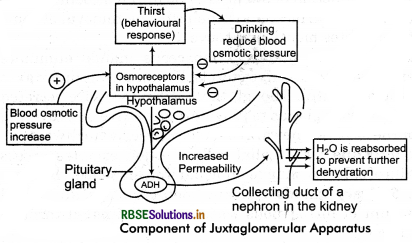
Human endocrine system play an important role in the regulation of kidney functions and a feedback control of urine formation. There are mainly two important hormonal controls of the kidney function by negative feedback circuit:
1. Control by Hypothalamus: When the blood osmolarity rises above the set point of 300 m osm/L, it stimulates the osmoreceptor cells of hypothalamus. These receptors respond by two methods:
(i) They promote thirst and thus drinking of water can reduce the osmolarity of blood.
(ii) Another response of osmoreceptor cells is release of antidiuretic hormone (ADH) by stimulating the posterior pituitary. This hormone makes the DCT more permeable to Na+. This increases the reabsorption of Na+ from DCT. The Na+ reabsorption promotes the passive reabsorption of water. In this way, more and more water is reabsorbed from DCT. This reabsorption helps in reduce the blood osmolarity. When the osmolarity blood becomes below 300 m osm/L, the hypothalamus stops the relase of ADH by pituitary (by feedback mechanism).
3 parts:
- Macula densa - cells of distal tubule.
- Juxtaglomerular (JG) cells modified smooth muscle cells (myoepithelioid) in arteriole.
- Extraglornerular mesangial.
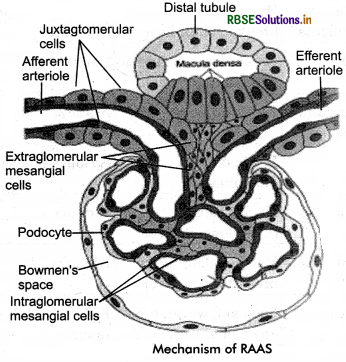
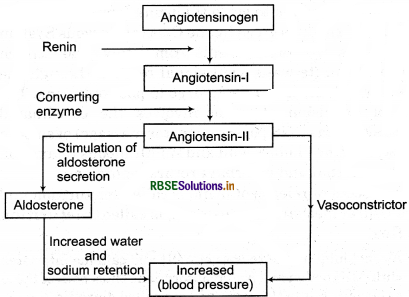
2. Control by Juxta Gtomerutar Apparatus or JGA: A fall in the blood pressure in afferent arteriole stimulate the cells of juxtaglomerular apparatus (described formerly) to release a hormone renin . Renin convert angiotensinogen (a plasma proteiñ formed in the liver) into angiotensin I (a peptide). This is further converted to angiotensin II by an enzyme ACE. Angiotensin II is a powerful vaso-constrictor and increases the blood volume (pressure) in two ways:
(i) It stimulates the PCT to reabsorb more Na+, Cl- and water.
(ii) It stimulate the adrenal gland to release aldosterone (a hormone that induces the DCT to reabsorb more Na and water). This multi hormonal mechanism operated by JGA is also called “Renin - Angiotensin - Aldosterone System (RAAS).
Regulation of Kidney Function by Heart Atrial Natri - uretic factor (a peptide hormone) produced from the walls of atria of heart opposes the RAAS mechanism (i.e., vasoconstriction). It is released in response to an increase in blood volume and pressure. ANF inhibit the release of renin from the JGA and thereby, inhibits Na+, Cl- and water reabsorption by the collecting duct. It also reduces the release of aldosterone from adrenal gland. ANF causes vasodilation (dilation of blood vessels) and thereby decreases the blood pressure.
